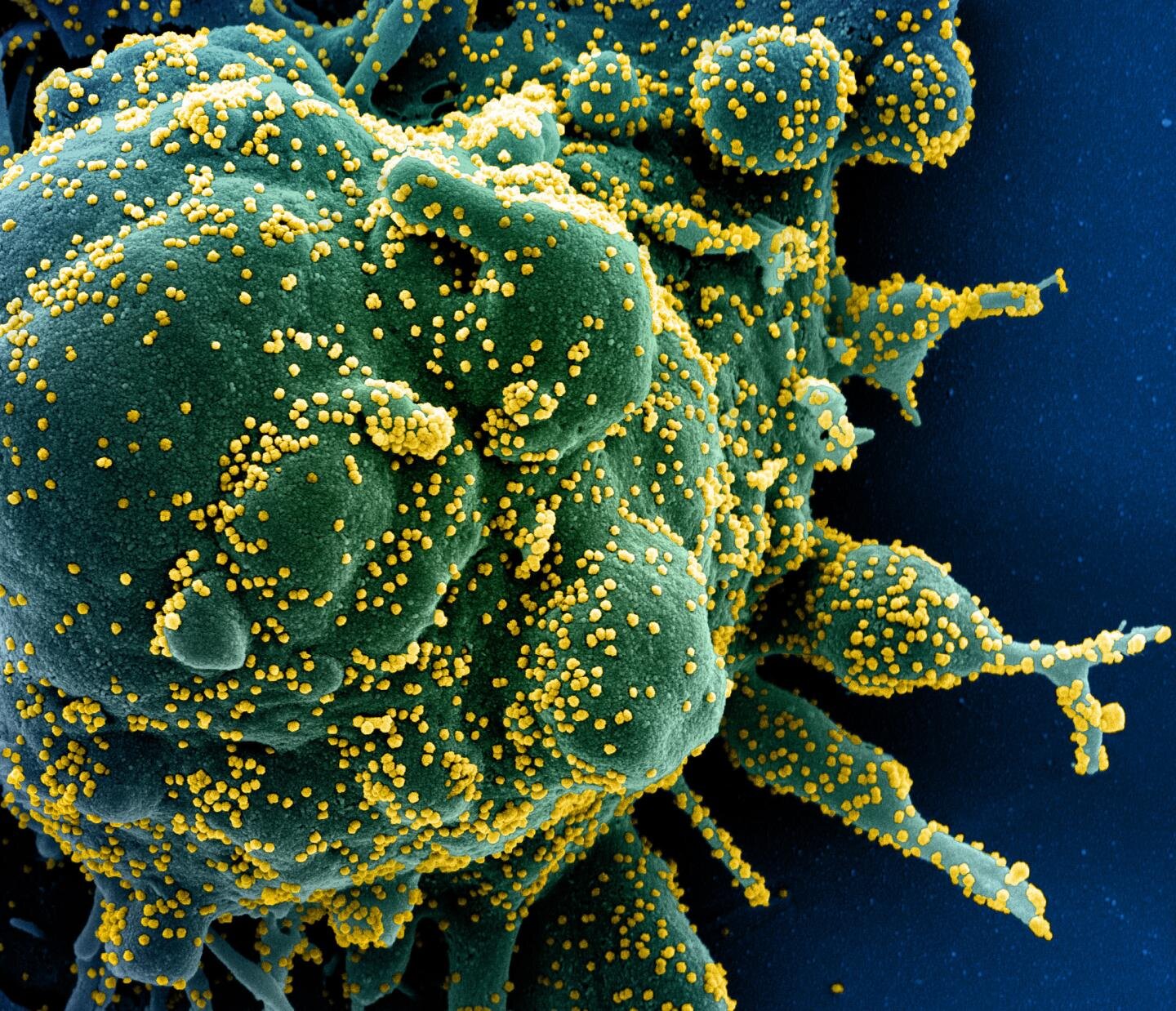
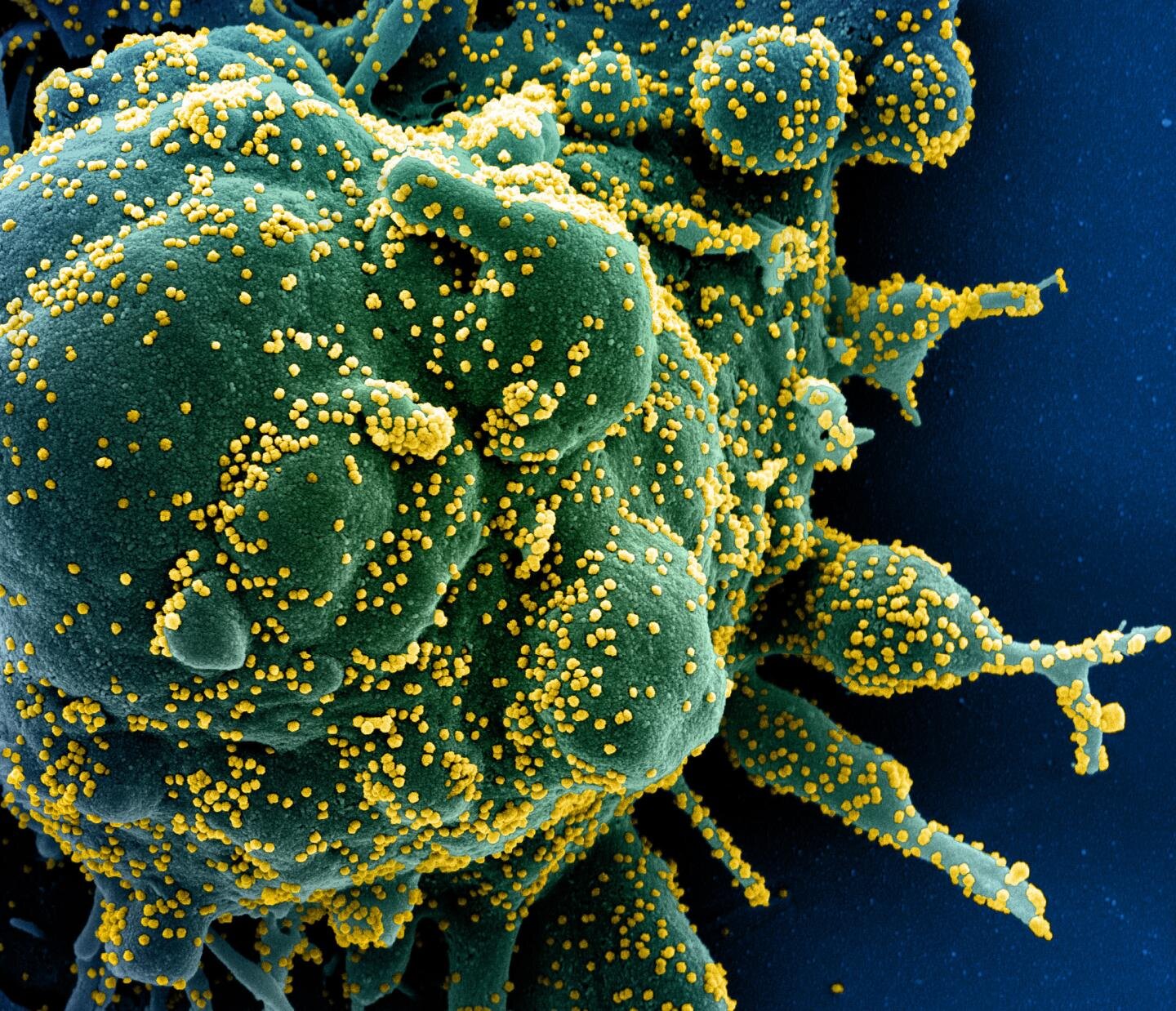
Johns Hopkins Medicine researchers have shown that it is possible for solid organ transplant recipients who contract COVID-19 to experience a natural immune response to SARS-CoV-2, the virus that causes the disease. In their study, published online Jan. 19, 2021, in the journal Transplantation, the researchers also suggest that measures used to provide short-term immunity against SARS-CoV-2—such as convalescent plasma (which contains antibodies from patients who have recovered from COVID-19)—may actually reduce the natural response.
“We followed 18 transplant recipients who were taking immunosuppressive medications to prevent rejection and who developed COVID-19 post-transplant,” says study co-author Dorry Segev, M.D., Ph.D., the Marjory K. and Thomas Pozefsky Professor of Surgery and Epidemiology and director of the Epidemiology Research Group in Organ Transplantation at the Johns Hopkins University School of Medicine. “Our goal was to gain a deeper understanding of the immune response in these individuals so that clinicians will be better able to treat transplant recipients who get COVID-19, prevent their disease from becoming severe and develop vaccine protocols that fit their special needs.”
The study participants, all of whom were receiving immunosuppressive medication, represented a variety of organ transplants: nine kidneys, five liver, one kidney and liver, two lungs and one composite tissue allograft (composed of different tissue types, such as skin, muscle, bone, bone marrow, lymph nodes, nerves and tendons). The median age was 56, 56% (10) were female, 33% (six) were Black and 11% (two) were Hispanic. COVID-19 occurred at a median of six years following transplant surgery, with 89% (16) experiencing symptoms and 72% (13) requiring hospitalization. Five patients received convalescent plasma during their hospital stay. When the participants were screened for SARS-CoV-2 antibodies at a median of 98 days after the COVID-19 diagnosis, the researchers observed that most had antibody levels suggesting neutralizing immunity—the ability to prevent reinfection if exposed to the virus in the future.
Transplant recipients who had more severe cases of COVID-19, the researchers say, tended to have the highest antibody levels.
Interestingly, the researchers found that transplant recipients who received convalescent plasma or intravenous immunoglobulin (to reduce the risk of a serious inflammatory response) had lower natural antibody levels against the virus and, therefore, were less likely to have immunity.
“This raises the possibility that administered antibody preparations may blunt the natural formation of antibodies against SARS-CoV-2,” says Jacqueline Garonzik Wang, M.D., Ph.D., associate professor of surgery at the Johns Hopkins University School of Medicine and study senior author. Larger studies will be needed to substantiate this finding, which, if proven, would be invaluable to COVID-19 vaccine protocol development for the immunocompromised.
more recommended stories
 Safer Allogeneic Stem Cell Transplants with Treg Therapy
Safer Allogeneic Stem Cell Transplants with Treg TherapyA new preclinical study from the.
 Autoimmune Disorders: ADA2 as a Therapeutic Target
Autoimmune Disorders: ADA2 as a Therapeutic TargetAdenosine deaminase 2 (ADA2) has emerged.
 Kaempferol: A Breakthrough in Allergy Management
Kaempferol: A Breakthrough in Allergy ManagementKaempferol, a dietary flavonoid found in.
 Early Milk Cereal Drinks May Spur Infant Weight Gain
Early Milk Cereal Drinks May Spur Infant Weight GainNew research published in Acta Paediatrica.
 TaVNS: A Breakthrough for Chronic Insomnia Treatment
TaVNS: A Breakthrough for Chronic Insomnia TreatmentA recent study conducted by the.
 First-of-Its-Kind Gene-Edited Pig Kidney: Towana’s New Life
First-of-Its-Kind Gene-Edited Pig Kidney: Towana’s New LifeSurgeons at NYU Langone Health have.
 Just-in-Time Training Improves Success & Patient Safety
Just-in-Time Training Improves Success & Patient SafetyA study published in The BMJ.
 ChatGPT Excels in Medical Summaries, Lacks Field-Specific Relevance
ChatGPT Excels in Medical Summaries, Lacks Field-Specific RelevanceIn a recent study published in.
 Study finds automated decision minimizes high-risk medicine combinations in ICU patients
Study finds automated decision minimizes high-risk medicine combinations in ICU patientsA multicenter study coordinated by Amsterdam.
 Study Discovers Connection Between Omicron Infection and Brain Structure Changes in Men
Study Discovers Connection Between Omicron Infection and Brain Structure Changes in MenA recent study in the JAMA.

Leave a Comment