AI (artificial intelligence) may appear to be a chilly robotic system, but Osaka Metropolitan University researchers have demonstrated that it may provide heartwarming—or, more specifically, “heart-warning”—support. They demonstrated a new use of artificial intelligence (AI) that classifies cardiac functions and pinpoints valvular heart disease with unparalleled precision, suggesting continuous progress in bridging the worlds of medicine and technology to improve patient treatment. The findings will appear in The Lancet Digital Health.
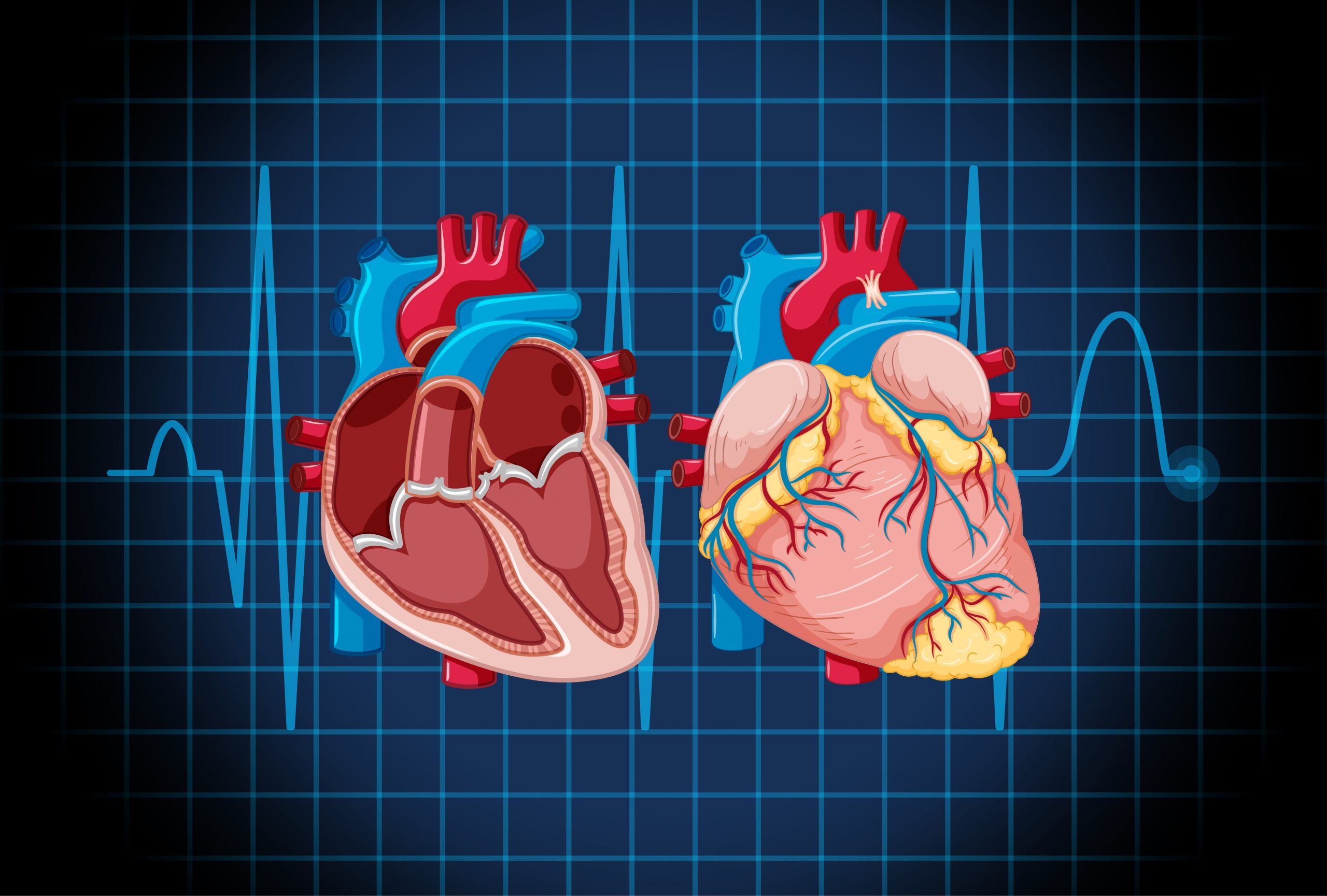
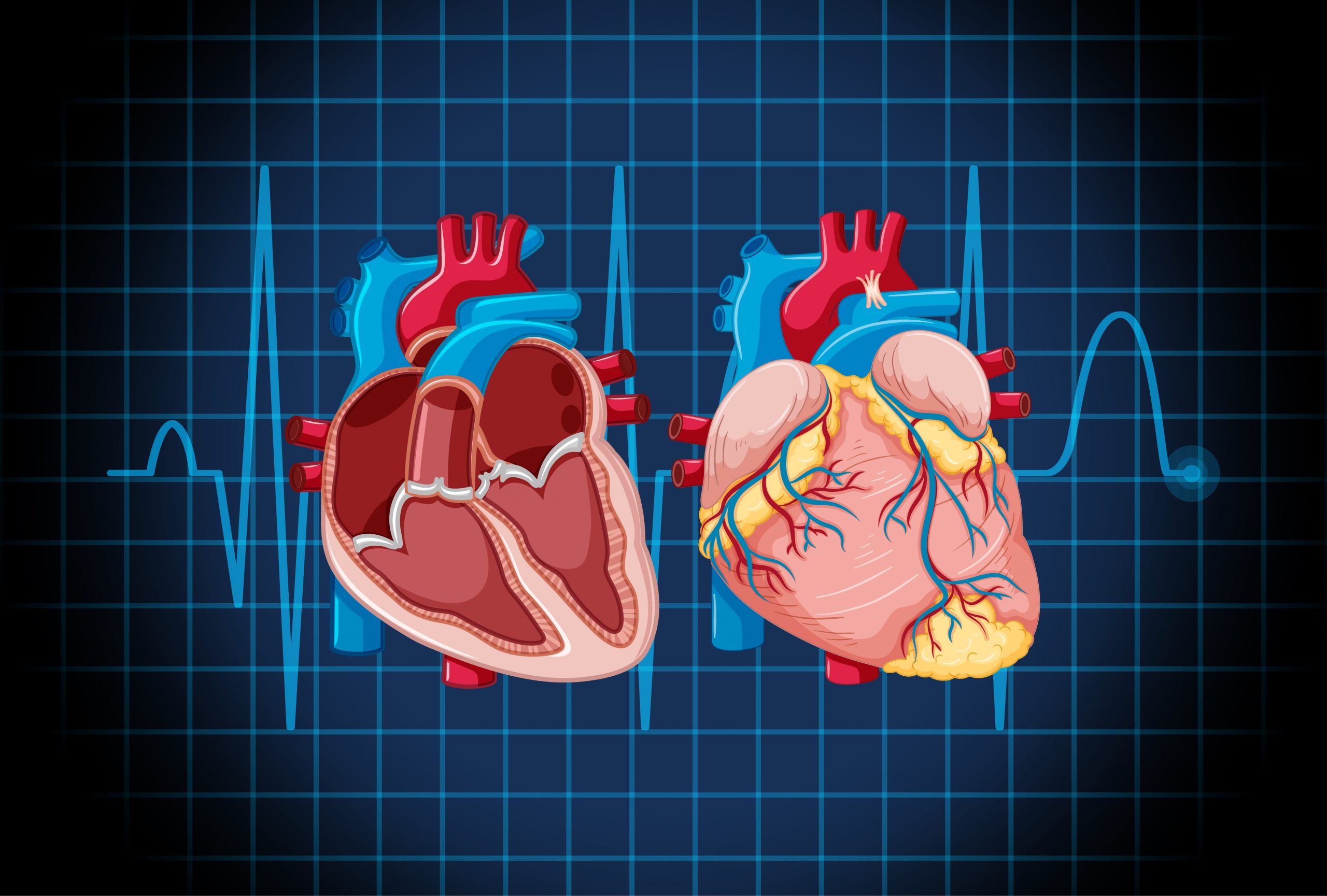
Echocardiography is frequently used to diagnose valvular heart disease, one of the leading causes of heart failure. However, because this approach demands specialized abilities, there is a corresponding shortage of skilled technicians. Meanwhile, chest radiography is one of the most commonly used techniques to diagnose disorders, particularly those of the lungs. Despite the fact that the heart can be seen in chest radiographs, nothing is known about the ability of chest radiographs to identify cardiac function or illness.
Chest radiographs, often known as chest X-rays, are conducted in many hospitals and take extremely little time to complete, making them very accessible and reproducible. As a result, the research team led by Dr. Daiju Ueda from the Department of Diagnostic and Interventional Radiology at Osaka Metropolitan University’s Graduate School of Medicine concluded that if cardiac function and disease could be determined from chest radiographs, this test could serve as a supplement to echocardiography.
Dr. Ueda’s team has created a model that uses artificial intelligence to effectively classify cardiac functions and valvular heart disorders from chest radiographs. Because AI trained on a single dataset may be biased, resulting in low accuracy, the researchers sought multi-institutional data.
As a result, between 2013 and 2021, a total of 22,551 chest radiographs and 22,551 echocardiograms were gathered from 16,946 individuals at four facilities. The AI model was trained to learn features connecting both datasets using chest radiographs as input data and echocardiograms as output data.
The AI model accurately classified six forms of valvular heart disease, with the Area Under the Curve, or AUC, ranging from 0.83 to 0.92. (AUC is a rating measure that reflects an AI model’s capability and uses a value range of 0 to 1, with the closer to 1, the better.) The AUC for detecting left ventricular ejection fraction—an important parameter for monitoring cardiac function—was 0.92 at a 40% cut-off.
“It took us a very long time to get to these results, but I believe this is significant research,” stated Dr. Ueda. “In addition to improving the efficiency of doctors’ diagnoses, the system might also be used in areas where there are no specialists, in night-time emergencies, and for patients who have difficulty undergoing echocardiography.”
more recommended stories
 Tuberculosis Breakthrough with Experimental Antibiotics
Tuberculosis Breakthrough with Experimental AntibioticsKey Takeaways Experimental antibiotics disrupt a.
 National Healthy Longevity Trial Receives Federal Support
National Healthy Longevity Trial Receives Federal SupportKey Summary Up to $38 million.
 Red Blood Cells Improve Glucose Tolerance Under Hypoxia
Red Blood Cells Improve Glucose Tolerance Under HypoxiaKey Takeaways for Clinicians Chronic hypoxia.
 Nanoplastics in Brain Tissue and Neurological Risk
Nanoplastics in Brain Tissue and Neurological RiskKey Takeaways for HCPs Nanoplastics are.
 AI Predicts Chronic GVHD Risk After Stem Cell Transplant
AI Predicts Chronic GVHD Risk After Stem Cell TransplantKey Takeaways A new AI-driven tool,.
 Red Meat Consumption Linked to Higher Diabetes Odds
Red Meat Consumption Linked to Higher Diabetes OddsKey Takeaways Higher intake of total,.
 Pediatric Crohn’s Disease Microbial Signature Identified
Pediatric Crohn’s Disease Microbial Signature IdentifiedKey Points at a Glance NYU.
 Nanovaccine Design Boosts Immune Attack on HPV Tumors
Nanovaccine Design Boosts Immune Attack on HPV TumorsKey Highlights Reconfiguring peptide orientation significantly.
 High-Fat Diets Cause Damage to Metabolic Health
High-Fat Diets Cause Damage to Metabolic HealthKey Points Takeaways High-fat and ketogenic.
 Acute Ischemic Stroke: New Evidence for Neuroprotection
Acute Ischemic Stroke: New Evidence for NeuroprotectionKey Highlights A Phase III clinical.

Leave a Comment