Weill Cornell Medicine and NewYork-Presbyterian researchers have found a startling mechanism that causes some lymphomas to be resistant to treatment.
The technique, which involves the movement of messenger RNAs (mRNAs) from the nucleus to the cytoplasm, ultimately helps cancer cells repair their DNA. As a result, these cancer cells can evade treatments that try to damage their DNA.
They established that a combination of approved chemotherapies, one of which targets the DNA repair-facilitating pathway, could help treat these persistent cases in a collaboration that included both fundamental research and clinical testing. While the study focused on diffuse large B-cell lymphoma (DLBCL), the findings are likely applicable to other cancer types as well.
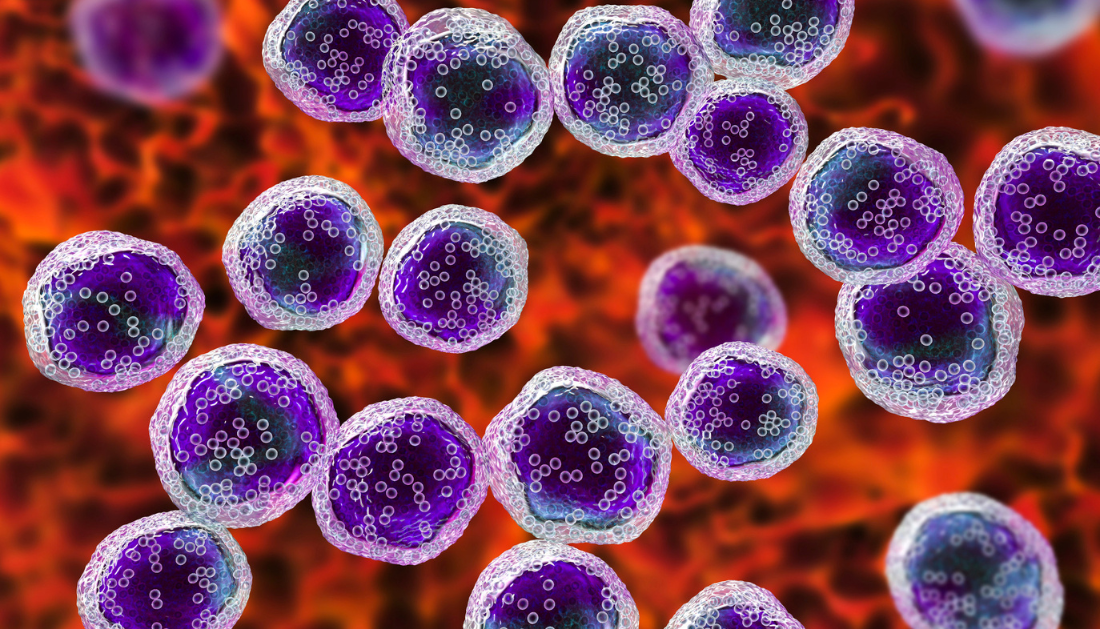
DLBCL is the most common type of lymphomas, affecting around 30,000 people in the United States alone each year. “But for people who aren’t cured or relapse, they historically had poor outcomes with standard chemotherapy-based treatment approaches,” said co-lead author Dr. Sarah Rutherford, an assistant professor of medicine at Weill Cornell Medicine and a hematologist/oncologist at NewYork-Presbyterian/Weill Cornell Medical Center.
Dr. Rossella Marullo, a teacher of medicine at Weill Cornell Medicine, is the other co-lead author.
Previous research has shown that treatment-resistant DLBCL cells frequently produce high quantities of a protein known as XPO1. In the year 2019, the U.S. The Food and medication Administration authorized selinexor, a novel medication designed to target XPO1 and block its function. The medicine is used to treat these refractory instances because it inhibits the proliferation of lymphoma cells that express high levels of the protein. Selinexor has helped many people with treatment-resistant illness, but not all.
“Selinexor is effective on its own; it’s just not as effective as we’d like it to be,” said Rutherford, who is also a member of Weill Cornell Medicine’s Sandra and Edward Meyer Cancer Center. This has motivated her to look for ways to improve the drug’s efficacy.
Meanwhile, Rutherford’s colleagues were attempting to discover more about the mechanism of action of selinexor. Its target, XPO1, moves hundreds of proteins and RNAs out of the cell nucleus, principally to separate the pool of proteins that should not be present, such as ribosomal proteins.
However, the researchers discovered that some of these XPO1-exported proteins are also attached to mRNA molecules, allowing these mRNAs to be exported from the cell nucleus into the cytoplasm and translated into proteins. According to this new mechanism, the amount and activity of XPO1 in a cell can thus impact the expression levels of multiple genes.
“We discovered that it’s not just regulating a few proteins, but it’s coordinating these big programs, allowing cells to rapidly adjust their proteome and survive different types of stress that cancer cells face all the time,” said senior author Dr. Leandro Cerchietti, the Richard Stratton Associate Professor of Hematology and Oncology and a member of Weill Cornell Medicine’s Meyer Cancer Center.
Using treatment-resistant DLBCL cells from patients and grafting them into preclinical models, the researchers discovered that increased levels of XPO1 eventually enhance the expression of genes that protect cells from death due to DNA damage. Inhibiting XPO1 with selinexor made the lymphomas more sensitive to DNA-damaging chemotherapies and immune-based treatments.
“We were excited, and based on some of Dr. Cerchietti’s research, we thought selinexor would likely synergize with other chemotherapies,” Rutherford said in a press release.
She launched a phase 1 clinical research to investigate whether such a combination would be safe in patients, and if so, at what doses. The research, which predominantly involved patients with treatment-resistant DLBCL, demonstrated that the combined regimen is not only safe, but also appears to be effective. Despite the fact that the dataset is too limited to make clear conclusions, several patients fared better than expected.
Rutherford is keen to test and refine the novel regimens in future trials. “It has been a really exceptional time over the last four years or so in this disease, where we now have many more therapies than we did when we first started the trial,” she told reporters.
Because XPO1 is expressed by every cell in the body, the new findings are likely to have broader implications. “There are other tumors in which XPO1 is overexpressed,” Cerchietti went on to say, “so it’s really a nice backbone to build on.”
This research was funded in part by the National Cancer Institute of the National Institutes of Health, the Leukemia & Lymphoma Society, and Karyopharm, Inc.
more recommended stories
 Phage Therapy Study Reveals RNA-Based Infection Control
Phage Therapy Study Reveals RNA-Based Infection ControlKey Takeaways (Quick Summary) Researchers uncovered.
 Safer Allogeneic Stem Cell Transplants with Treg Therapy
Safer Allogeneic Stem Cell Transplants with Treg TherapyA new preclinical study from the.
 AI in Emergency Medicine and Clinician Decision Accuracy
AI in Emergency Medicine and Clinician Decision AccuracyEmergency teams rely on rapid, accurate.
 Innovative AI Boosts Epilepsy Seizure Prediction by 44%
Innovative AI Boosts Epilepsy Seizure Prediction by 44%Transforming Seizure Prediction in Epilepsy Seizure.
 Hypnosis Boosts NIV Tolerance in Respiratory Failure
Hypnosis Boosts NIV Tolerance in Respiratory FailureA New Approach: Hypnosis Improves NIV.
 Bee-Sting Microneedle Patch for Painless Drug Delivery
Bee-Sting Microneedle Patch for Painless Drug DeliveryMicroneedle Patch: A Pain-Free Alternative for.
 AI Reshapes Anticoagulation in Atrial Fibrillation Care
AI Reshapes Anticoagulation in Atrial Fibrillation CareUnderstanding the Challenge of Atrial Fibrillation.
 Hemoglobin as Brain Antioxidant in Neurodegenerative Disease
Hemoglobin as Brain Antioxidant in Neurodegenerative DiseaseUncovering the Brain’s Own Defense Against.
 Global Data Resource for Progressive MS Research (Multiple Sclerosis)
Global Data Resource for Progressive MS Research (Multiple Sclerosis)The International Progressive MS Alliance has.
 AI Diabetes Risk Detection: Early T2D Prediction
AI Diabetes Risk Detection: Early T2D PredictionA new frontier in early diabetes.

Leave a Comment