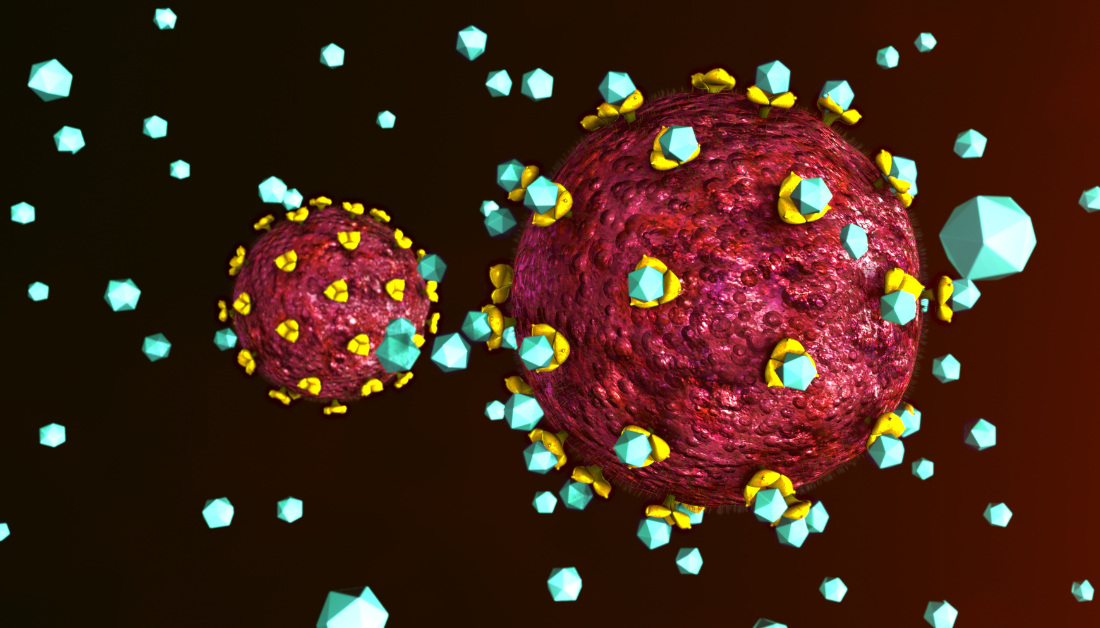
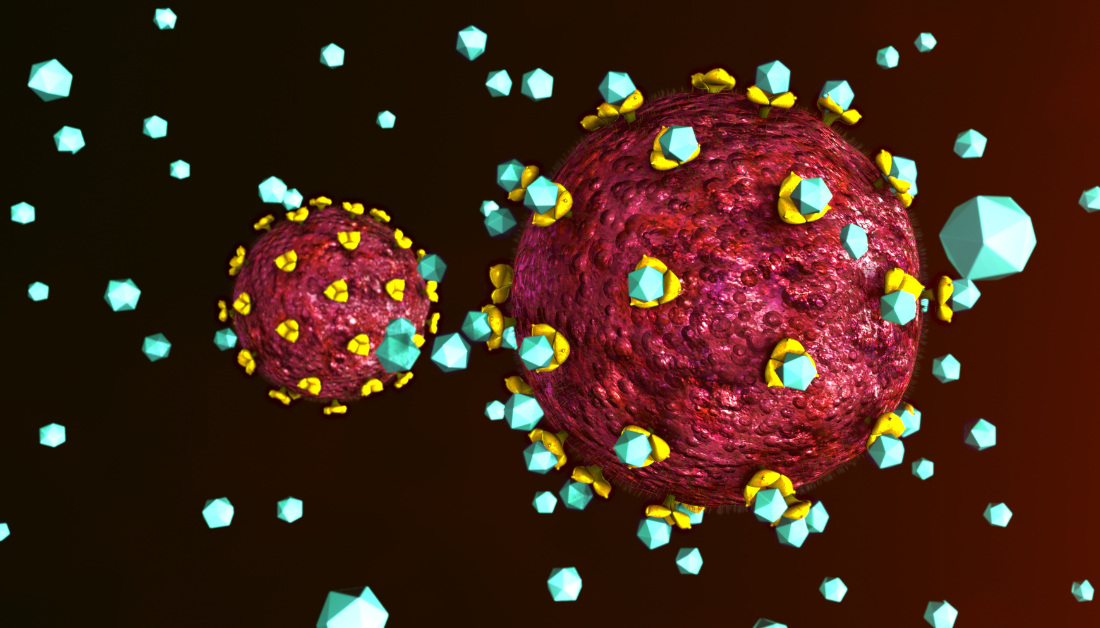
A recent study in EBioMedicine analyzed the effects of nicotinamide mononucleotide (NMN) on CD4+ Thymus cells (T cells), which are T lymphocytes with CD4 receptors, and their role in immune activation during HIV-1 infection.
Background
In HIV-1 infections, approximately 30% of people undergoing combination antiretroviral therapy (cART) fail to adequately restore CD4+ T cells, increasing their susceptibility to immune deficiency syndromes (AIDS) and associated illnesses.
Research indicates that Vitamin D and Vitamin B3 (niacin), which are known to enhance Nicotinamide adenine dinucleotide (NAD) – crucial for cell metabolism and declining with age – are effective in immune modulation and supporting the restoration of CD4+ T cells. NMN, a direct NAD precursor without the adverse effects of other precursors, shows promise as a treatment for age-related conditions and for enhancing immune responses to infections and cancer.
Additional research is required because, despite the effectiveness of cART in reducing HIV-1 viremia, a significant number of individuals do not recover their CD4+ T cell count, leading to higher clinical risks. Understanding the role of NMN in modulating immune activation could provide new strategies for enhancing CD4+ T cell recovery and reducing disease progression in these patients.
About the study
In this study, researchers utilized peripheral blood from both HIV-1-uninfected donors and people living with HIV (PLWH) to isolate peripheral blood mononuclear cells (PBMCs). They employed Lymphoprep™ for density gradient centrifugation and various isolation techniques to minimize cell activation.
The isolated PBMCs and primary CD4+ T cells were cultured in R10 medium and modified for NMN treatment experiments. The HIV-1JRFL virus was propagated using the MOLT-4 CCR5+ cell line for virus preparation and infection, while the Human Embryonic Kidney 293 cells with a transfection receptor (HEK293T) cell line were used for packaging a non-replicable HIVJRFL-nLuc pseudovirus.
Researchers used a spinoculation technique to introduce these viruses into primary CD4+ T cells and the MOLT-4 CCR5+ cell line. They incorporated various control measures, such as mock infections and pre-treatment with Maraviroc, to ensure rigorous experimentation. Reactivation of the virus in ex vivo primary cell models and cell lines was achieved through specific treatments.
The MOLT-4 CCR5+ cells underwent cell transfection, followed by NMN treatment and RNA extraction. Mycoplasma-free cell lines played a crucial role in various assays, including anti-p24 Enzyme-Linked Immunosorbent Assay (ELISA) and luciferase assays, to measure NAD levels, cell viability, and pseudotyped virus responses. DNA and RNA extractions were conducted after NMN treatment or HIV-1 infection, with quantitative real-time PCR assays providing in-depth analysis.Flow cytometry was utilized for cell surface and intracellular staining.
The study also included experiments on humanized mice, with careful consideration of animal welfare and experimental conditions. The team monitored the mice’s plasma viral loads and cellular markers, collecting spleen samples for additional research. Advanced methods like Cytometry by Time-Of-Flight (CyTOF), Immunohistochemistry (IHC) staining, and RNA sequencing were used to assess the impact of NMN treatment at a molecular level. The research concluded with thorough statistical analyses and adherence to ethical standards, upholding research integrity.
Study results
For more information: Nicotinamide mononucleotide impacts HIV-1 infection by modulating immune activation in T lymphocytes and humanized mice. EBioMedicine.
more recommended stories
 Nanoplastics in Brain Tissue and Neurological Risk
Nanoplastics in Brain Tissue and Neurological RiskKey Takeaways for HCPs Nanoplastics are.
 AI Predicts Chronic GVHD Risk After Stem Cell Transplant
AI Predicts Chronic GVHD Risk After Stem Cell TransplantKey Takeaways A new AI-driven tool,.
 Red Meat Consumption Linked to Higher Diabetes Odds
Red Meat Consumption Linked to Higher Diabetes OddsKey Takeaways Higher intake of total,.
 Pediatric Crohn’s Disease Microbial Signature Identified
Pediatric Crohn’s Disease Microbial Signature IdentifiedKey Points at a Glance NYU.
 Nanovaccine Design Boosts Immune Attack on HPV Tumors
Nanovaccine Design Boosts Immune Attack on HPV TumorsKey Highlights Reconfiguring peptide orientation significantly.
 High-Fat Diets Cause Damage to Metabolic Health
High-Fat Diets Cause Damage to Metabolic HealthKey Points Takeaways High-fat and ketogenic.
 Acute Ischemic Stroke: New Evidence for Neuroprotection
Acute Ischemic Stroke: New Evidence for NeuroprotectionKey Highlights A Phase III clinical.
 Statins Rarely Cause Side Effects, Large Trials Show
Statins Rarely Cause Side Effects, Large Trials ShowKey Points at a Glance Large.
 Anxiety Reduction and Emotional Support on Social Media
Anxiety Reduction and Emotional Support on Social MediaKey Summary Anxiety commonly begins in.
 Liquid Biopsy Measures Epigenetic Instability in Cancer
Liquid Biopsy Measures Epigenetic Instability in CancerKey Takeaways Johns Hopkins researchers developed.

Leave a Comment