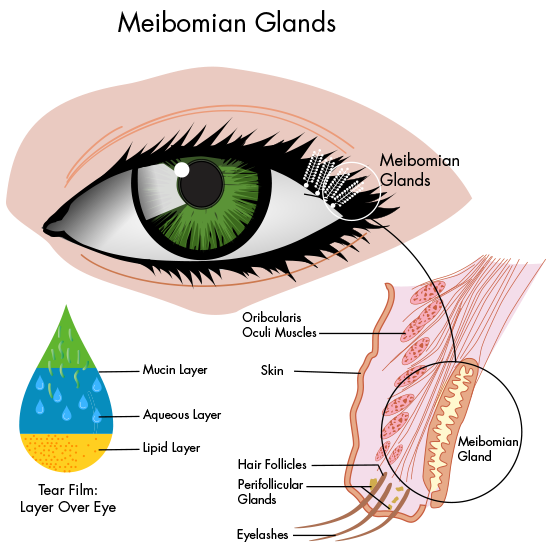
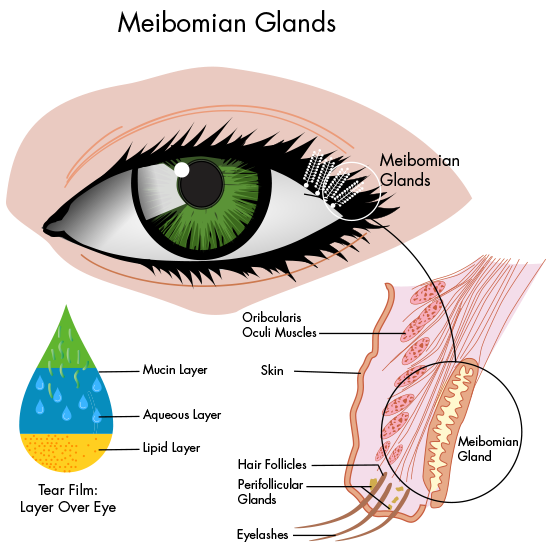
Meibomian Gland Dysfunction (MGD) is a mainly obstructive Dysfunction of the Lipid-producing Meibomian Glands (termed ´Obstructive MGD´) inside the tarsal plates of the eye lids that leads to a Lack of Lipids with resulting Tear Film Deficiency and Evaporative Dry Eye Disease.
Due to the obstruction of lipid outflow from the gland, it also causes a pressure atrophy of the gland inside the eye lid with dilatation of the ductal system and atrophy of the secretory acini.
MGD is sub-summarized under BLEPHARITIS – as the main type of posterior Blepharitis.
Meibomian gland dysfunction (MGD) is the most frequent cause of dry eye disease (DED). In fact, more than 86% of patients with DED are noted to have meibomian gland dysfunction.
Meibomian glands, to the best of our knowledge, do not regenerate once destroyed. Therefore, the need to identify and treat MGD early is of the utmost importance. Studies have also shown the potential negative effect untreated MGD can have on the accuracy of preoperative measurements in cataract surgery.
Our understanding of the pathophysiology of MGD has evolved considerably over the past several years. The original DEWS study established evaporative DED associated with MGD was far more common than aqueous-deficient DED.
Baudouin et al postulated that the underlying pathophysiological mechanisms of DED and MGD interact, resulting in a self-perpetuating “double vicious circle” causing a disruption in tear film homeostasis.
The International Workshop on Meibomian Gland Dysfunction established a standard definition of MGD in 2011: “Meibomian gland dysfunction (MGD) is a chronic, diffuse abnormality of the meibomian glands, commonly characterized by terminal duct obstruction and/or qualitative/quantitative changes in the glandular secretion.
This may result in alteration of the tear film, symptoms of eye irritation, clinically apparent inflammation, and ocular surface disease.”
A greater understanding of the disease process has led to a growing number of treatment options available for patients.
Much like dental hygiene, to be successful in treatment of MGD, patients must take an active role in caring for their glands with daily in-home therapies that can be enhanced by more advanced in-office procedures.
AT-HOME TREATMENTS
At a minimum, patients with MGD should be encouraged to perform routine warm compresses at home. Studies have shown that the melting point of the meibum appears to be increased from 32°C in normal patients to 35°C in MGD patients.
The application of heat to the eyelids at a minimum effective temperature of 41.5°C promotes melting of the meibum and consequent unplugging of the gland orifices to normalize flow of the oil into the tear film.
At home, heat can simply be applied via a number of methods, from a hot wash cloth to a rice bag. However, compliance with this treatment can be difficult to achieve (both in time required and maintenance of temperature).
In our practice, we have found that utilizing a commercially made heated eye mask such as the Bruder Moist Heat Eye Compress or The Eye Doctor Premium Moist Heat Compress helps improve patient compliance with this step.
Lid hygiene with baby shampoo or lid scrub pads goes hand in hand with warm compresses. It is also an important component of the overall treatment plan when addressing MGD associated with Demodex.
Potential beneficial at-home lid hygiene treatments include the use of lid cleansers with tea tree oil (TheraTears SteriLid eyelid cleanser), cleansing pads (Cliradex towelettes, Blephadex Eyelid Foam [Lunovus]) and hypochlorous acid spray (Avenova, Bruder) to reduce bacterial load on the eyelids.
Other potential at-home treatments include NuLids (NuSight Medical), which patients may use to help clean the eyelids and massage the glands.
It consists of a disposable silicone tip which can be coupled with a cleanser and used to gently clean off any scurf or debris, signaling 15 seconds per lid for a total of one minute of care.
In addition, prescription anti-inflammatory drops such as cyclosporine (Restasis, Allergan; Cequa, Sun Ophthalmics) or lifitegrast (Xiidra, Novartis) may also be used, as both have been shown to potentially aid in the treatment of MGD, as well as loteprednol etabonate ophthalmic suspension 0.25% (Eysuvis, Kala Pharmaceuticals).
If patients present with MGD in association with rosacea, low dose oral doxycycline should also be considered for its anti-inflammatory and lipid regulating properties.
In addition, we have found topical azithromycin 1% to be a useful adjunct in treatment of MGD, especially when associated with staphylococcal blepharitis.
Further, though the role of Omega-3 supplementation for MGD has been met with controversy after the results of the DREAM study, many ophthalmologists find use of high quality supplements to benefit their patients.
IN-OFFICE PROCEDURES
In-office procedures to treat MGD can range from manual expression of meibomian glands to more technologically advanced approaches, such as debridement scaling, intraductal probing, thermal pulsation and intense pulsed light therapy.
Physical expression of meibomian glands at the slit lamp has been utilized for more than 90 years. Despite the pain associated with it, a number of studies demonstrate its efficacy.
Depending on the level of anterior blepharitis present, debridement scaling may be appropriate as well.
In our experience, we have found combining thermal heat with gland expression to be the most effective, long-term, in-office procedure that I am able to offer patients for treatment of MGD.
A number of devices are available for thermal heating and expression of the glands; however, there are nuances that make each device unique.
Given the high prevalence of MGD as a cause of DED and its deleterious effects, early identification and treatment of MGD should not be overlooked. As a chronic disease, it is important to educate patients on the important role they play in long term treatment of disease.
Incorporating advanced office-based treatments will allow for greater success in management of the disease, thereby improving patient outcomes long term.
more recommended stories
 Diabetic Kidney Disease: Combo Therapy Targets Zombie Cells
Diabetic Kidney Disease: Combo Therapy Targets Zombie CellsKey Points Researchers from Mayo Clinic.
 Heart Attack Recovery: Single Injection May Heal the Heart
Heart Attack Recovery: Single Injection May Heal the HeartKey Points Researchers have developed a.
 Fragmentome Technology Detects Early Liver Fibrosis
Fragmentome Technology Detects Early Liver FibrosisKey Points at a Glance AI-based.
 CTNNB1 Syndrome Study Explores Beta-Catenin Defects
CTNNB1 Syndrome Study Explores Beta-Catenin DefectsKey Takeaways Researchers in Spain are.
 Tuberculosis Breakthrough with Experimental Antibiotics
Tuberculosis Breakthrough with Experimental AntibioticsKey Takeaways Experimental antibiotics disrupt a.
 National Healthy Longevity Trial Receives Federal Support
National Healthy Longevity Trial Receives Federal SupportKey Summary Up to $38 million.
 Red Blood Cells Improve Glucose Tolerance Under Hypoxia
Red Blood Cells Improve Glucose Tolerance Under HypoxiaKey Takeaways for Clinicians Chronic hypoxia.
 Nanoplastics in Brain Tissue and Neurological Risk
Nanoplastics in Brain Tissue and Neurological RiskKey Takeaways for HCPs Nanoplastics are.
 AI Predicts Chronic GVHD Risk After Stem Cell Transplant
AI Predicts Chronic GVHD Risk After Stem Cell TransplantKey Takeaways A new AI-driven tool,.
 Red Meat Consumption Linked to Higher Diabetes Odds
Red Meat Consumption Linked to Higher Diabetes OddsKey Takeaways Higher intake of total,.

Leave a Comment