

A global observational study conducted by UCL (University College London) including over 3,200 newborn babies suffering from sepsis in 19 hospitals in 11 countries found that many newborns are dying because the antibiotics used to treat sepsis are losing their effectiveness.
The study, which lasted from 2018 to 2020, discovered a high mortality rate among newborns with culture-positive sepsis (almost 1 in 5 across hospital sites) as well as a considerable burden of antibiotic resistance. The study produced a plethora of high-quality data that will be used to improve the care of newborns with sepsis.
The findings of the observational study were published in a report in PLOS Medicine by a multinational team of over 80 researchers from four continents.
The Global Antibiotic Research and Development Partnership (GARDP) conducted the study in collaboration with the Medical Research Council Clinical Trials Unit at UCL, whose research team led the data analysis; St George’s, University of London (SGUL); Penta—Child Health Research; and the University of Antwerp.
“It was very important to undertake this study to get a better understanding of the kind of infections we’re seeing in newborns in hospitals, the bugs causing them, the treatments that are being used and why we are seeing more deaths. The study has given us vital information which will help us to better design clinical trials and ultimately improve the care and outcome of babies with neonatal sepsis,” said Manica Balasegaram, Executive Director of GARDP.
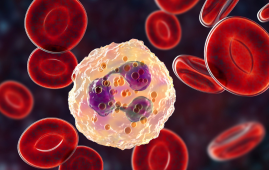
Sepsis is a potentially fatal bloodstream illness that affects up to 3 million newborns worldwide each year. Every year, 214,000 newborn newborns, predominantly in low- and middle-income countries (LMICs), die of antibiotic-resistant sepsis. Because of their immature immune systems, newborn newborns are especially vulnerable to serious illness.
Findings
Mortality rates ranged from 1.6% to 27.3% among the 19 hospitals in the research, with LMICs having much higher rates. The study included leading clinicians from hospitals in Bangladesh, Brazil, China, Greece, India, Italy, Kenya, South Africa, Thailand, Vietnam, and Uganda.
“The study exposed the glaring reality of antibiotic-resistant infections, especially in hospitals in LMICs, where we are often faced with a shortage of nurses, beds and space. The risk of infections is very high and most infections are resistant to antibiotics. If an antibiotic doesn’t work, the baby often dies. This urgently needs to change. We need antibiotics that will cover all bacterial infections,” said Sithembiso Velaphi, head of pediatrics at Chris Hani Baragwanath Academic Hospital in Johannesburg, South Africa.
The study reveals an alarmingly broad difference in treatment. In the study, hospitals utilized over 200 different antibiotic combinations, with frequent antibiotic change due to significant resistance to treatments.
Because of the high level of antibiotic resistance to the recommended therapies in their units, many physicians were forced to utilize antibiotics such as carbapenems. The World Health Organization classifies these as “Watch” antibiotics. They are only suggested for certain, limited indications since they must be conserved. However, these medicines were frequently the only ones available to treat the infection.
Last-line antibiotics were given to 15% of the neonates in the study who had neonatal sepsis. Klebsiella pneumoniae was the most commonly isolated pathogen. It is frequently linked to hospital-acquired illnesses.
Steps to improve treatment and survival in the future
Using the information gathered, the researchers created two tools that could be utilized in clinical trials and in any newborn intensive care unit across the world. Clinicians might use the NeoSep Severity Score, which is based on 10 clinical signs and symptoms, to identify babies who are at high risk of dying and ensure they receive special attention more promptly. Many of the same clinical indications and symptoms are used in the NeoSep Recovery Score, which could give clinicians with critical information on whether to escalate treatment.
“The observational study has been instrumental in providing the high-quality data that we need to design trials of appropriate treatments for sepsis in newborn babies. It has been a huge collaborative effort by researchers and clinicians in Africa, Asia, Latin America and Europe,” said Neal Russell, Principal Investigator for the neonatal sepsis study at SGUL.
The study also aims to inform WHO guidelines on infant sepsis therapy.
“Organisms evolve, drug resistance changes; that is why clinical guidelines for neonatal sepsis need constant adaptation. Updating guidelines relies on recent and good evidence, so this observational study is a significant step towards better treatment,” said Wolfgang Stöhr, statistician for the observational study at the MRC Clinical Trials Unit at UCL.
The study’s findings were used to create a crucial strategic public health clinical trial to find better treatments for neonatal infections in the setting of rising resistance to present treatments.
The newborn sepsis study (NeoSep1) is being done at Chris Hani Baragwanath Academic Hospital in Soweto, Johannesburg, Tygerberg Hospital in Cape Town, and Kilifi County Hospital in Kenya, and is being lead by GARDP in collaboration with SGUL and the MRC CTU at UCL. The experiment will also investigate the best formulations and dosages for newborn newborns. From 2024, the experiment will be expanded to other countries and regions, with a goal of recruiting up to 3,000 babies in total.
“Work in formulation and dose appropriateness is imperative. Children are not small adults. Drugs must be formulated to meet their needs in a safe and effective manner,” said Alessandra Nardone, Clinical Project Manager at Penta—Child Health Research.
The new trial will benefit from the observational study’s crucial laboratory work.
more recommended stories
 Silica Nanomatrix Boosts Dendritic Cell Cancer Therapy
Silica Nanomatrix Boosts Dendritic Cell Cancer TherapyKey Points Summary Researchers developed a.
 Vagus Nerve and Cardiac Aging: New Heart Study
Vagus Nerve and Cardiac Aging: New Heart StudyKey Takeaways for Healthcare Professionals Preserving.
 Cognitive Distraction From Conversation While Driving
Cognitive Distraction From Conversation While DrivingKey Takeaways (Quick Summary) Talking, not.
 Fat-Regulating Enzyme Offers New Target for Obesity
Fat-Regulating Enzyme Offers New Target for ObesityKey Highlights (Quick Summary) Researchers identified.
 Spatial Computing Explains How Brain Organizes Cognition
Spatial Computing Explains How Brain Organizes CognitionKey Takeaways (Quick Summary) MIT researchers.
 Gestational Diabetes Risk Identified by Blood Metabolites
Gestational Diabetes Risk Identified by Blood MetabolitesKey Takeaways (Quick Summary for Clinicians).
 Phage Therapy Study Reveals RNA-Based Infection Control
Phage Therapy Study Reveals RNA-Based Infection ControlKey Takeaways (Quick Summary) Researchers uncovered.
 Pelvic Floor Disorders: Treatable Yet Often Ignored
Pelvic Floor Disorders: Treatable Yet Often IgnoredKey Takeaways (Quick Summary) Pelvic floor.
 Urine-Based microRNA Aging Clock Predicts Biological Age
Urine-Based microRNA Aging Clock Predicts Biological AgeKey Takeaways (Quick Summary) Researchers developed.
 Circadian Control of Neutrophils in Myocardial Infarction
Circadian Control of Neutrophils in Myocardial InfarctionKey Takeaways for HCPs Neutrophil activity.

Leave a Comment