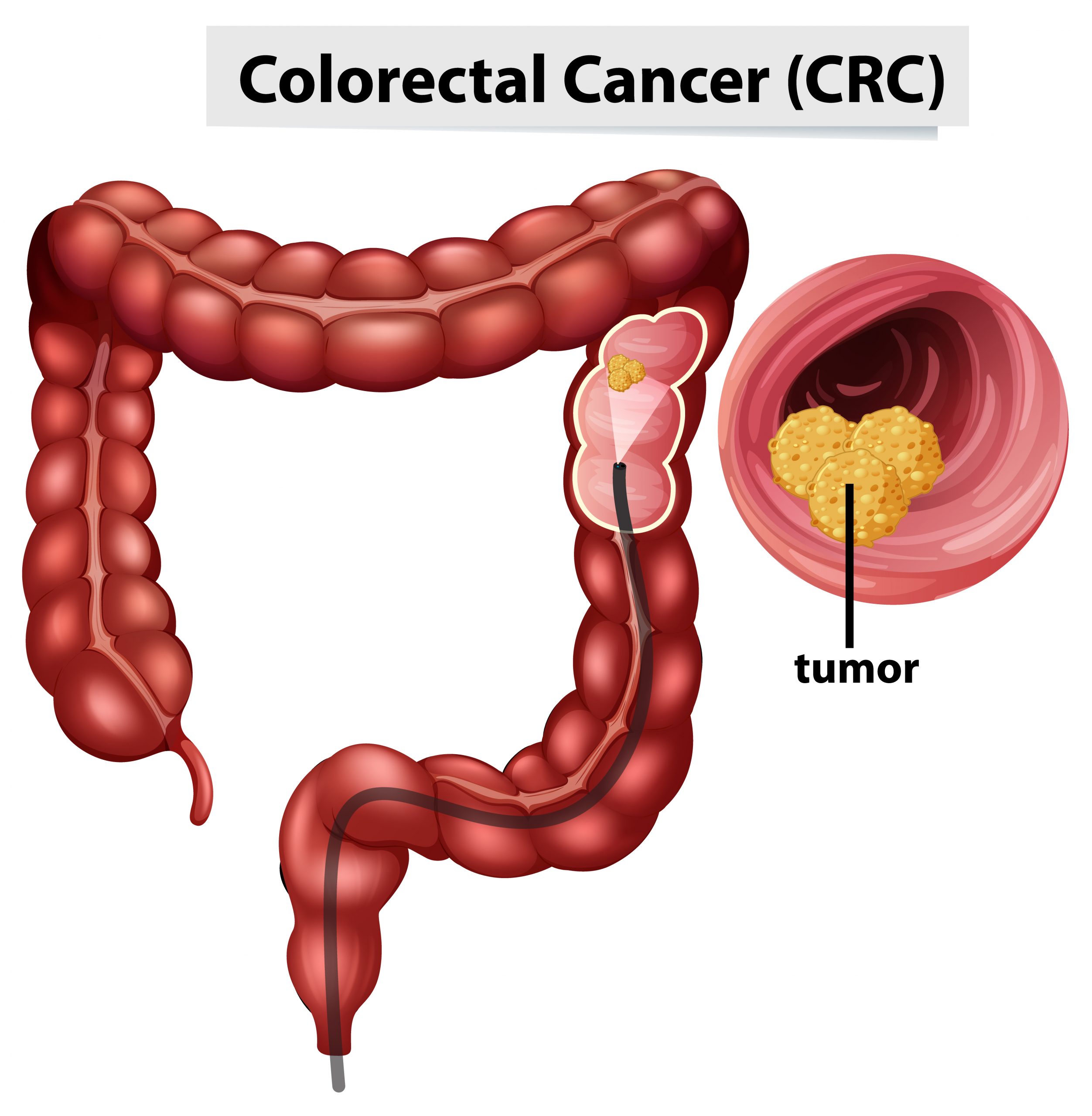
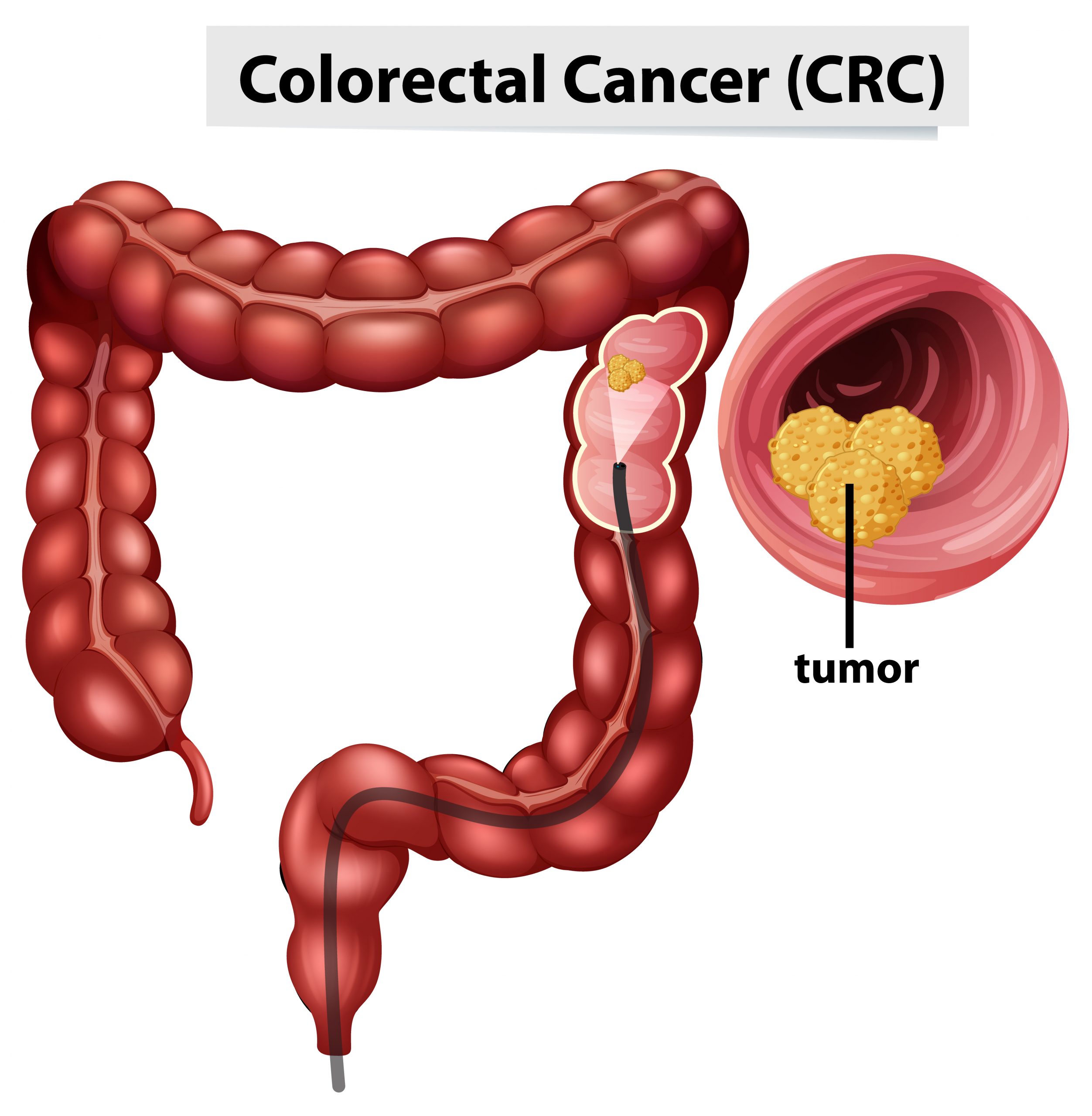
When cancer spreads to other parts of the body (known as metastasis), it becomes more difficult to cure. This is especially true in cases of colorectal cancer that has progressed to the liver. Some patients with limited metastases, on the other hand, can achieve long-term survival, and even cure, if they are treated with intensive localized therapies like surgery or radiation therapy.
Researchers at the University of Chicago Medicine Comprehensive Cancer Center are now utilizing a novel method they created to predict which patients with metastatic colorectal cancer would have a favorable treatment outcome (prognosis) following surgical excision of liver metastases. The strategy entails combining a panel of genetic biomarkers with clinical tumor traits to identify various subgroups of cancer that correspond to varied treatment results. On July 20, 2023, the findings were published in JAMA Oncology.
The new study builds on work published in Nature Communications in 2018 by Sean P. Pitroda, MD, Ralph R. Weichselbaum, MD, and colleagues, who discovered unique molecular patterns that identified patients with a favorable subtype of colorectal liver metastases who experienced long post-surgery survival rates.
In the United Kingdom, molecular profiling was performed on 147 colorectal cancer patients with limited liver metastasis who were treated with chemotherapy and surgery in a large, multicenter phase 3 randomized clinical trial called New-EPOC to validate a novel biomarker panel consisting of 31 genes. The panel was created at the University of Chicago using mathematical modeling, which resulted in 96% accuracy in identifying the disease’s molecular subtype.
“Combining biological data with clinical features strongly predicted a patient’s risk of metastasis recurrence and survival following treatment,” said Pitroda, corresponding author of the paper and Associate Professor of Radiation and Cellular Oncology at the University of Chicago Medicine.
Oligometastasis of colorectal cancer
The “oligometastasis” hypothesis, introduced by UChicago physician-scientists Samuel Hellman, MD, and Ralph R. Weichselbaum, MD in 1995, states that cancer spreads along a continuum from a few to many sites.
The oligometastasis concept implies that malignancies with limited dissemination in the body (usually one to five locations) can be eradicated by local interventions such as surgery or radiation, whereas traditional palliative therapies like as chemotherapy fail to eradicate metastatic illness.
“Over the past 30 years, the oligometastasis hypothesis has been supported by numerous clinical studies and revolutionized the treatment of metastatic disease,” said Pitroda. “Although curative therapies were shown to be promising, only 20% to 30% of patients with limited metastasis demonstrated long-term survival, indicating the critical need for biomarkers that could identify which patients derive the largest benefit from localized interventions, such as surgery.”
Molecular pattern discovery
Prior to this study, UChicago researchers worked with colleagues at NorthShore University Health System, Evanston Hospital, to undertake a retrospective sequencing analysis on metastatic liver tissues to find genetic patterns underlying the disparities in patient outcomes. They discovered three unique molecular patterns based on messenger RNA (mRNA) and microRNA (miRNA) expression profiles that classified metastases as canonical, immunological, or stromal.
The immunological subtype had the best prognosis out of the three. The immunological subtype’s tumor microenvironment appeared to activate an immune response in the liver, which may have helped to limit fresh tumor growth and produce improved treatment outcomes.
When the scientists linked genetic subtypes with clinical characteristics, they discovered three integrated risk categories with dramatically different 10-year survival rates of 94%, 45%, and 19% for low-risk, intermediate-risk, and high-risk patients, respectively.
“Despite these promising results, we needed to validate our findings in an independent, prospectively collected clinical dataset before we can incorporate the three molecular subtypes into our clinical practice,” said Pitroda.
Molecular subtype validation
Researchers collected molecular profile data from 93 individuals treated at the University of Chicago Medical Center in Hyde Park for the current investigation. They used an artificial intelligence neural network classifier to predict the disease’s molecular subtype. This group was referred to as a discovery cohort.
The researchers uncovered 31 genes that correctly predicted the molecular subtype 96% of the time. The neural network classifier was subsequently used to an independent set of 147 New-EPOC trial patients known as the validation cohort.
“When the molecular subtypes were combined with clinical features like tumor size and lymph node involvement, it strongly predicted the patient’s prognosis,” said Pitroda.
In contrast to the intermediate-risk (60% survival) and high-risk (40% survival) categories, patients with low-risk disease had an outstanding chance of surviving (80% at five years).
The importance of the work
The Ludwig Center for Metastasis Research at the University of Chicago is dedicated to understanding the biology of metastasis, and this study contributes to that objective, according to Pitroda.
We now have the first validated oligometastasis biomarker for predicting outcomes for patients with colorectal cancer spread to the liver. Our findings provide a novel framework for staging and classifying metastasis, which could lead to improved personalized therapy for patients by optimally integrating both local and systemic interventions,” said Pitroda.
“Although we have conducted these studies in colorectal cancer metastasis, a similar approach could be applied to other types of cancer. We believe this will challenge the way we currently treat metastatic disease and open new opportunities to design future clinical trials and improve outcomes for our patients,” he added.
more recommended stories
 Red Blood Cells Improve Glucose Tolerance Under Hypoxia
Red Blood Cells Improve Glucose Tolerance Under HypoxiaKey Takeaways for Clinicians Chronic hypoxia.
 Nanoplastics in Brain Tissue and Neurological Risk
Nanoplastics in Brain Tissue and Neurological RiskKey Takeaways for HCPs Nanoplastics are.
 AI Predicts Chronic GVHD Risk After Stem Cell Transplant
AI Predicts Chronic GVHD Risk After Stem Cell TransplantKey Takeaways A new AI-driven tool,.
 Red Meat Consumption Linked to Higher Diabetes Odds
Red Meat Consumption Linked to Higher Diabetes OddsKey Takeaways Higher intake of total,.
 Pediatric Crohn’s Disease Microbial Signature Identified
Pediatric Crohn’s Disease Microbial Signature IdentifiedKey Points at a Glance NYU.
 Nanovaccine Design Boosts Immune Attack on HPV Tumors
Nanovaccine Design Boosts Immune Attack on HPV TumorsKey Highlights Reconfiguring peptide orientation significantly.
 High-Fat Diets Cause Damage to Metabolic Health
High-Fat Diets Cause Damage to Metabolic HealthKey Points Takeaways High-fat and ketogenic.
 Acute Ischemic Stroke: New Evidence for Neuroprotection
Acute Ischemic Stroke: New Evidence for NeuroprotectionKey Highlights A Phase III clinical.
 Statins Rarely Cause Side Effects, Large Trials Show
Statins Rarely Cause Side Effects, Large Trials ShowKey Points at a Glance Large.
 Anxiety Reduction and Emotional Support on Social Media
Anxiety Reduction and Emotional Support on Social MediaKey Summary Anxiety commonly begins in.

Leave a Comment