When we perform cataract surgery for patients with retinal disease, we must tailor the IOL type, design and power to maximize vision given the underlying pathology.
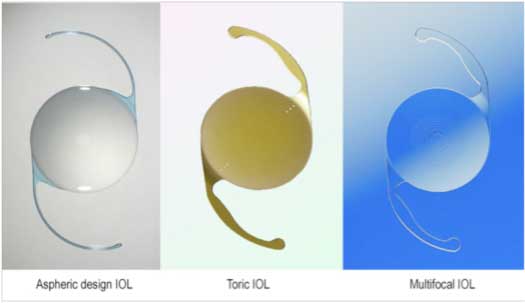
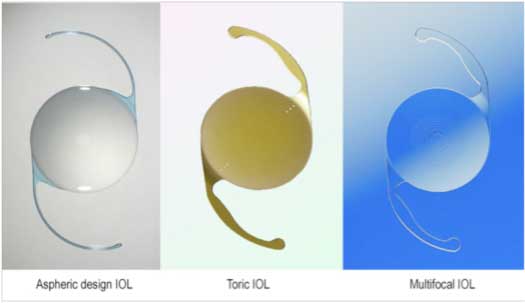
The IOL type that we will most often utilize is a monofocal optic, with or without toric correction. We will sometimes prefer a three-piece IOL design because it will give more options for placement or future suture fixation. For the IOL power consideration, a target of Plano or mild myopia is typically recommended, with care taken to adjust the dioptric strength based on the anticipated effective lens position.
For patients with
For patients with extreme myopia, cataract surgery can be a great blessing because we can correct 20 D of refractive error at the same time. We must first ensure that the retinal periphery is stable and without breaks and that the macula is free from pathology. When we replace the 4-mm thick cataractous lens with the new 1-mm thin IOL, there will be a shift of vitreous, which may induce a posterior vitreous detachment. This shifting vitreous can also place stress on the retinal periphery and can induce a retinal break or even detachment. For this reason, these patients should have their retinas examined in the postoperative period. With extreme axial myopia, lifetime follow-up with a retina specialist is recommended because the development of some degree of retinal pathology is almost certain in the future.
Retinitis pigmentosa
Patients with the progressive disease retinitis pigmentosa tend to develop cataracts at an early age. There are also special considerations for their cataract surgery because they are at higher risk of capsular phimosis due to weakened zonular support and of cystoid macular edema due to chronic inflammation. Monofocal IOLs are the best choice in these patients with a target of about Plano. In some cases, three-piece IOL designs are favored because they provide more options for suture fixation in the future if there is a dislocation of the IOL-bag complex. Capsular tension rings may also be useful in some cases, and patients should be treated with topical anti-inflammatory medications for an extended period of time. While a toric IOL can be a good option for patients with a significant degree of corneal astigmatism, we should avoid using light-splitting optic designs, which can decrease contrast.
Post-pars plana vitrectomy
After performing a vitrectomy, particularly if intravitreal gas is used, a cataract tends to develop in the next year or so. If a white cataract develops within the first month after the pars plana vitrectomy, there may be a compromise of the lens capsule. This is rare, and most patients develop a nuclear cataract more gradually. While performing cataract surgery in a post-vitrectomy eye, there is less support of the crystalline lens due to the loss of vitreous and lack of anterior hyaloid face support. When we implant the IOL, we can also expect that the effective lens position will be slightly more posterior, and therefore we should increase the IOL power slightly, usually by about 0.5 D. Monofocal IOLs tend to be the best choice, particularly if there is a history of macular pathology. Three-piece IOL designs may offer more options for placement in cases of compromised zonular support.
Retinal vascular disease
The most common retinal vascular diseases that we see are related to diabetes and hypertension. These disease processes tend to occur slowly over the course of years, but acute conditions such as retinal vein occlusion can happen suddenly. Cataract surgery should be delayed until the retinal disease is treated and stabilized. Patients with preexisting macular edema may end up with more fluid accumulation and worse retinal status after cataract surgery. In addition, even when the underlying retinal vascular disease is quiescent, the retinal status may not return to normal levels. This makes placing a light-splitting lens, such as diffractive multifocal or extended depth of focus designs, a suboptimal choice. For most of these patients, a monofocal IOL with a target of about Plano is the best option.
A significant portion of our cataract surgery patients have underlying retinal pathology, and we should tailor the IOL selection and technique of phacoemulsification to their condition. In most cases, this means a monofocal IOL and a target of Plano to mild myopia. While we may not be able to return these patients to perfect vision due to the preexisting retinal disease, we can greatly improve their vision with cataract surgery and the appropriate IOL choice.
more recommended stories
 Safer Allogeneic Stem Cell Transplants with Treg Therapy
Safer Allogeneic Stem Cell Transplants with Treg TherapyA new preclinical study from the.
 Autoimmune Disorders: ADA2 as a Therapeutic Target
Autoimmune Disorders: ADA2 as a Therapeutic TargetAdenosine deaminase 2 (ADA2) has emerged.
 Kaempferol: A Breakthrough in Allergy Management
Kaempferol: A Breakthrough in Allergy ManagementKaempferol, a dietary flavonoid found in.
 Early Milk Cereal Drinks May Spur Infant Weight Gain
Early Milk Cereal Drinks May Spur Infant Weight GainNew research published in Acta Paediatrica.
 TaVNS: A Breakthrough for Chronic Insomnia Treatment
TaVNS: A Breakthrough for Chronic Insomnia TreatmentA recent study conducted by the.
 First-of-Its-Kind Gene-Edited Pig Kidney: Towana’s New Life
First-of-Its-Kind Gene-Edited Pig Kidney: Towana’s New LifeSurgeons at NYU Langone Health have.
 Just-in-Time Training Improves Success & Patient Safety
Just-in-Time Training Improves Success & Patient SafetyA study published in The BMJ.
 ChatGPT Excels in Medical Summaries, Lacks Field-Specific Relevance
ChatGPT Excels in Medical Summaries, Lacks Field-Specific RelevanceIn a recent study published in.
 Study finds automated decision minimizes high-risk medicine combinations in ICU patients
Study finds automated decision minimizes high-risk medicine combinations in ICU patientsA multicenter study coordinated by Amsterdam.
 Study Discovers Connection Between Omicron Infection and Brain Structure Changes in Men
Study Discovers Connection Between Omicron Infection and Brain Structure Changes in MenA recent study in the JAMA.

Leave a Comment