

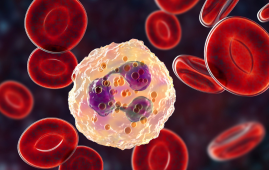
Panvascular illnesses are a newly recognized term for a set of cardiac conditions that primarily manifest as atherosclerosis and affect vital organs like the heart, brain, kidneys, and limbs. Hypoxia-inducible factor (HIF) is a crucial regulator of how the cardiovascular system reacts to everyday stressors like hypoxia.
Vascular smooth muscle cells (VSMCs) are important cells that control the pressure in the circulatory system and the transport of oxygen. In-depth research is necessary due to the plasticity, adaptability, and interactions of these two components with panvascular disorders.
HIFs are closely linked to overactive or defective VSMCs in the pathological state of panvascular disorders, including atherosclerosis, pulmonary arterial hypertension, and vascular calcification. These pervasive systemic illnesses highlight the multidisciplinary approach of panvascular medicine.
The delicate balance between angiogenesis and cancer progression, as well as the similar proliferative traits of VSMCs and cancer cells, highlight the urgent need for more precise regulatory targets or combination therapies to boost the efficacy of HIF-targeted therapies.
Considering the relevance of balancing global and local, as well as temporal and spatial elements, this review focuses on evaluating the significance of the HIF signaling pathway in panvascular disorders associated to VSMCs based on the aforementioned material.
The review also considered the advantages and disadvantages of HIF-related therapeutic targets in panvascular disorders. A brand-new class of medication called “-dustats” can inhibit PHD and hence activate the HIF-EPO pathway while having a mild influence on the body’s production of EPO. The medicine “-dustats” has been shown in previous research to enhance iron metabolism while treating anemia, and it typically does not exhibit major cardiovascular side effects or encourage the development of cancer.
Additionally, more effective direct activation targeting the specific HIF isoforms or more precise and focused indirect activation of HIF (e.g., inhibitors targeting specific PHD1-3 or FIH) are also required for more precise and targeted HIF pathway-activating medicines. Drug resistance is another issue that needs to be addressed.
In order to advance the transformation of HIF-related therapeutic approaches for VSMC in panvascular medicine, it is important to consider the following three factors:
(1) Emphasizing the HIFs’ shared and distinct roles in panvascular illness;
(2) The general thought of concentrating on HIF-related pathways, and
(3) The creation of precise medications that target pathways connected to HIF.
Overall, the clinical transformation of HIFs-related therapies necessitates that researchers explore and clarify the various roles and interactions of HIFs in different organs/systems or different stages of the disease, pharmaceutical experts or engineers work to industrialize the production of personalized therapies, and doctors pay more attention to individual differences (e.g., place of residence, gender, and disease) in diagnosis and treatment to identify underlying problems.
It is therefore possible to realize the significant clinical transformation of HIFs-related treatment in panvascular medicine based on the tenet of “from doctors, by engineers/researchers, for patients.”
Science Bulletin, a journal, published the research. Professors Junbo Ge, Hua Li, and Hao Lu from the Department of Cardiology at Zhongshan Hospital, Fudan University, and the Shanghai Institute of Cardiovascular Diseases respectively served as the study’s principal investigators.
more recommended stories
 Vagus Nerve and Cardiac Aging: New Heart Study
Vagus Nerve and Cardiac Aging: New Heart StudyKey Takeaways for Healthcare Professionals Preserving.
 Cognitive Distraction From Conversation While Driving
Cognitive Distraction From Conversation While DrivingKey Takeaways (Quick Summary) Talking, not.
 Fat-Regulating Enzyme Offers New Target for Obesity
Fat-Regulating Enzyme Offers New Target for ObesityKey Highlights (Quick Summary) Researchers identified.
 Spatial Computing Explains How Brain Organizes Cognition
Spatial Computing Explains How Brain Organizes CognitionKey Takeaways (Quick Summary) MIT researchers.
 Gestational Diabetes Risk Identified by Blood Metabolites
Gestational Diabetes Risk Identified by Blood MetabolitesKey Takeaways (Quick Summary for Clinicians).
 Phage Therapy Study Reveals RNA-Based Infection Control
Phage Therapy Study Reveals RNA-Based Infection ControlKey Takeaways (Quick Summary) Researchers uncovered.
 Pelvic Floor Disorders: Treatable Yet Often Ignored
Pelvic Floor Disorders: Treatable Yet Often IgnoredKey Takeaways (Quick Summary) Pelvic floor.
 Urine-Based microRNA Aging Clock Predicts Biological Age
Urine-Based microRNA Aging Clock Predicts Biological AgeKey Takeaways (Quick Summary) Researchers developed.
 Circadian Control of Neutrophils in Myocardial Infarction
Circadian Control of Neutrophils in Myocardial InfarctionKey Takeaways for HCPs Neutrophil activity.
 E-Cigarette Use and Heart Attack Risk in Former Smokers
E-Cigarette Use and Heart Attack Risk in Former SmokersKey Takeaways for Clinicians and Nurses.

Leave a Comment