Low testosterone in men is a condition that is more common today than many people may think. Over two-hundred thousand (200,000) males in the United States are diagnosed with a testosterone deficiency every year according to the most recent statistics. This condition of low testosterone is also frequently referred to as H.
Basically, the condition is caused by a decrease in a man’s functional activity of his testes that results in a reduction of his normal testosterone production. A normal part of aging in men is this decline in testosterone levels. The decline on average is roughly estimated to be about one percent annually after the age of 40. Most older men still have testosterone levels within the normal range, with only an estimated 10 -25% having levels considered to be low. Low testosterone levels in older men may therefore often go unnoticed.
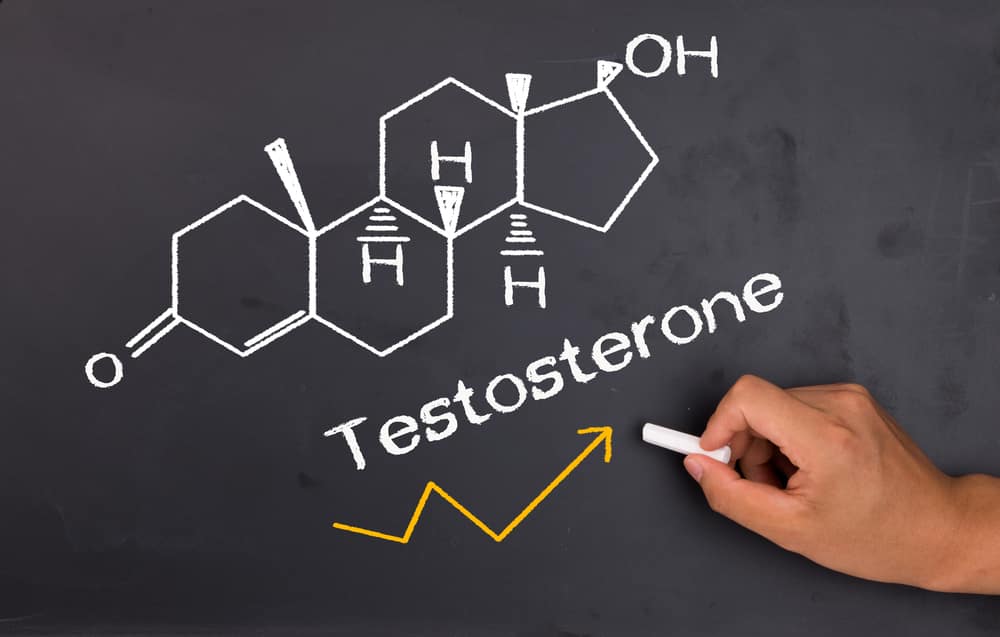
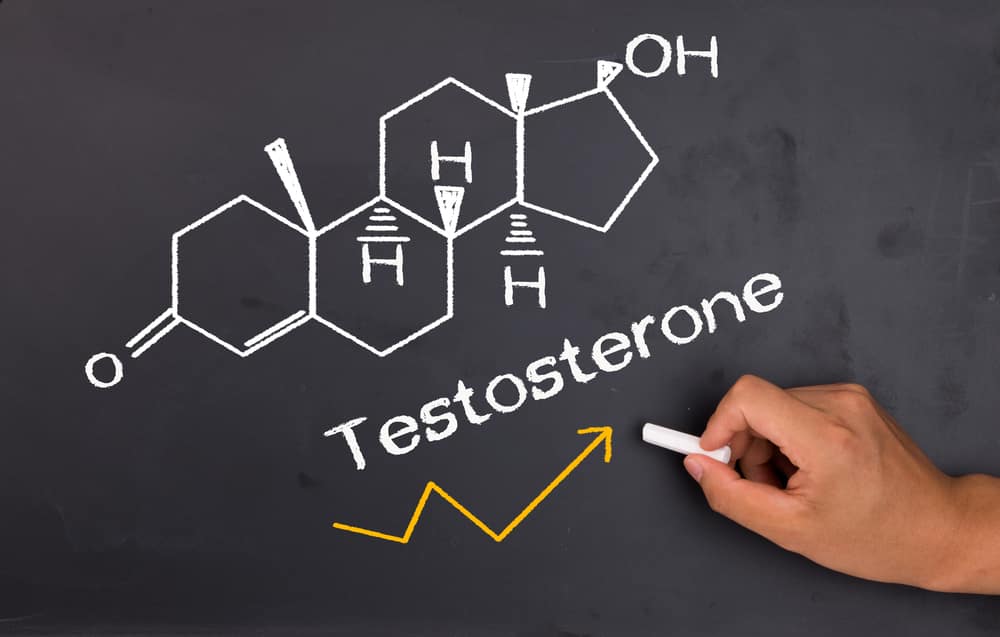
Testosterone is a type of male steroid hormone that a man’s testicles normally produce (although some is also produced by the man’s adrenal glands). It basically is a male hormone that provides a lot of “what makes a man a man” in both the physical and mental sense (please note that women create testosterone also, but at much reduced levels). The testosterone is responsible for both stimulating and regulating the normal development in men of their sexual maturation, leading to the onset of puberty and production of sperm. Along with then maintaining a man’s sexual drive, libido and performance, testosterone additionally helps maintain an individual’s muscle and bone density, red blood cell production and energy levels. It is also closely tied to a man’s cardiovascular health (his heart and blood vessels), and low testosterone levels have been documented to result in an increased potential for cardiovascular problems and even higher mortality rates in males.
Causes and Symptoms of Low Testosterone
Although primarily seen in men over the age of 40 (with the highest occurrence in men 60+ years of age or more), low testosterone can afflict a male at just about any age. In a normal man, his testosterone reaches its highest level during his early adulthood, then begins to gradually decline by an estimated one percent (1%) annually as a part of the normal aging process. This gradual decrease in male hormones (or androgens) seen in the normal aging process with men is sometimes called “male menopause “or “manopause” or referred to as late-onset hypogonadism (LOH).
In certain cases, the low testosterone can be congenital, or present at birth. Rare genetic disorders such as CHARGE syndrome, Hereditary Hemochromatosis or Klinefelter syndrome (one of the most common chromosomal disorders that occurs in about two out of one-hundred male babies) are characterized by hypogonadism. Additionally, there are other circumstances that can result in a man having low testosterone levels:
– In what is called Opioid Induced Androgen Deficiency, a low testosterone level may be the result of prolonged use of opioid drugs and painkillers (such as morphine, codeine, hydrocodone, oxycodone, hydromorphone and methadone).
– The long-term use of anabolic steroids by men can lead to a condition known as ASIH or anabolic-induced hypogonadism
– Childhood mumps
– Traumatic brain injury
Symptoms of low testosterone levels in a man may include:
– Lowered libido or a decrease in a man’s “sex drive” or sexual desire
– Chronic fatigue and low energy levels
– Erectile dysfunction
– Loss of muscle mass
– Decreased sleep or sleep deprivation
– A diminished mental cognition functionality such as reduced understanding and comprehension
– Reduced body hair and beard growth
– Enlarged breasts (known as gynecomastia)
Treatments for Low Testosterone Levels in Men
The condition of a low testosterone level can only be diagnosed by a physician, but it is easily identified by using a simple blood test. It’s best if the blood test is taken in the early morning when the patient’s T levels are the highest, as the blood levels can drop by up to thirteen percent (13%) later in the day.
Treatments are based on the replacement of the testosterone in order to restore a patient’s T levels back to normal, thus resulting in improvement and a decrease in the symptoms associated with having a low T level. Normal T blood levels will obviously depend on an individual man’s age, but they can range between approximately 240 nanograms/deciliter to upwards of 1,000 nanograms/deciliter. When a patient is exhibiting symptoms and their T levels are at the low end of the scale, then testosterone replacement therapy may be a viable option. Treatment is often prescribed for patients where their total testosterone level is below 300 nanograms/deciliter with symptoms being present.
It is important to be aware that testosterone replacement treatment does not take the place of initiating a proper diet, and both an exercise plan and a weight loss plan by the patient. These will assist in any treatment chosen for the patient’s Low T and help lead to better cardiovascular health.
Testosterone Replacement Therapy
Testosterone replacement therapies are also quite frequently called “T replacement therapy” for short and can include the following treatment methods:
– Topical Applications – Applied transdermally (absorbed through the patient’s skin) by using a patch or applying a topical cream or gel. Some of the major brands are AndroGel, Axiron, Testim and Fortesta.
– Injections – Treatment usually starts with an initial intramuscular injection of testosterone by a physician, which is then repeated every two weeks. There are also long acting injectables available that can last up to ten weeks after administration.
– Pellets – These are designed to deliver testosterone after administration to a patient for three to four months or longer. Known commonly as TESTOPEL, a rather simple procedure performed by a trained urologist at their office takes only about fifteen minutes. These offer the advantage of being a long-acting treatment solution, versus the daily application of a cream or a two to ten-week repeated injection. Additionally, they are not transferable to others as the topical applications can be.
– Oral – JATENZO® (testosterone undecanoate) is the first and only FDA-approved oral softgel for testosterone replacement therapy (TRT). It’s important to note that the oral use of testosterone was not available in the US until the FDA approved the use of JATENZO in early 2019.
A patient must also understand that testosterone replacement treatments take time and sometimes an immediate effect is not seen. Positive results may take as long as two to three months to begin to see a significant reduction in a patient’s symptoms. Additionally, treatment requires consistent evaluation by a doctor to ensure that the testosterone level in the patient’s blood is increasing adequately and that the treatment is working as expected.
more recommended stories
 Anxiety Reduction and Emotional Support on Social Media
Anxiety Reduction and Emotional Support on Social MediaKey Summary Anxiety commonly begins in.
 Liquid Biopsy Measures Epigenetic Instability in Cancer
Liquid Biopsy Measures Epigenetic Instability in CancerKey Takeaways Johns Hopkins researchers developed.
 Human Antibody Drug Response Prediction Gets an Upgrade
Human Antibody Drug Response Prediction Gets an UpgradeKey Takeaways A new humanized antibody.
 Pancreatic Cancer Research: Triple-Drug Therapy Success
Pancreatic Cancer Research: Triple-Drug Therapy SuccessKey Summary Spanish researchers report complete.
 Immune Cell Epigenome Links Genetics and Life Experience
Immune Cell Epigenome Links Genetics and Life ExperienceKey Takeaway Summary Immune cell responses.
 Dietary Melatonin Linked to Depression Risk: New Study
Dietary Melatonin Linked to Depression Risk: New StudyKey Summary Cross-sectional analysis of 8,320.
 Chronic Pain Linked to CGIC Brain Circuit, Study Finds
Chronic Pain Linked to CGIC Brain Circuit, Study FindsKey Takeaways University of Colorado Boulder.
 New Insights Into Immune-Driven Heart Failure Progression
New Insights Into Immune-Driven Heart Failure ProgressionKey Highlights (Quick Summary) Progressive Heart.
 Microplastic Exposure and Parkinson’s Disease Risk
Microplastic Exposure and Parkinson’s Disease RiskKey Takeaways Microplastics and nanoplastics (MPs/NPs).
 Sickle Cell Gene Therapy Access Expands Globally
Sickle Cell Gene Therapy Access Expands GloballyKey Summary Caring Cross and Boston.

Leave a Comment