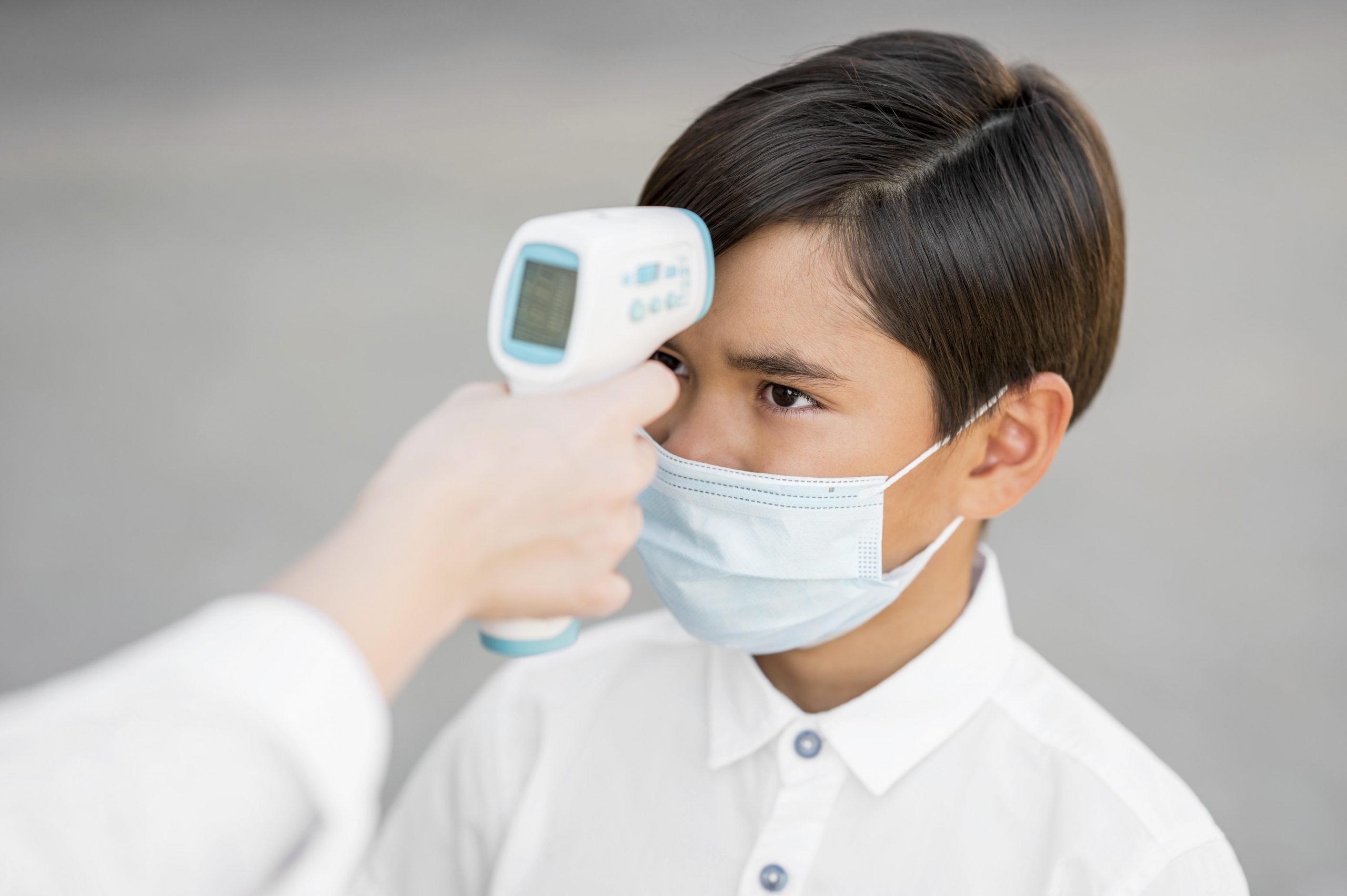
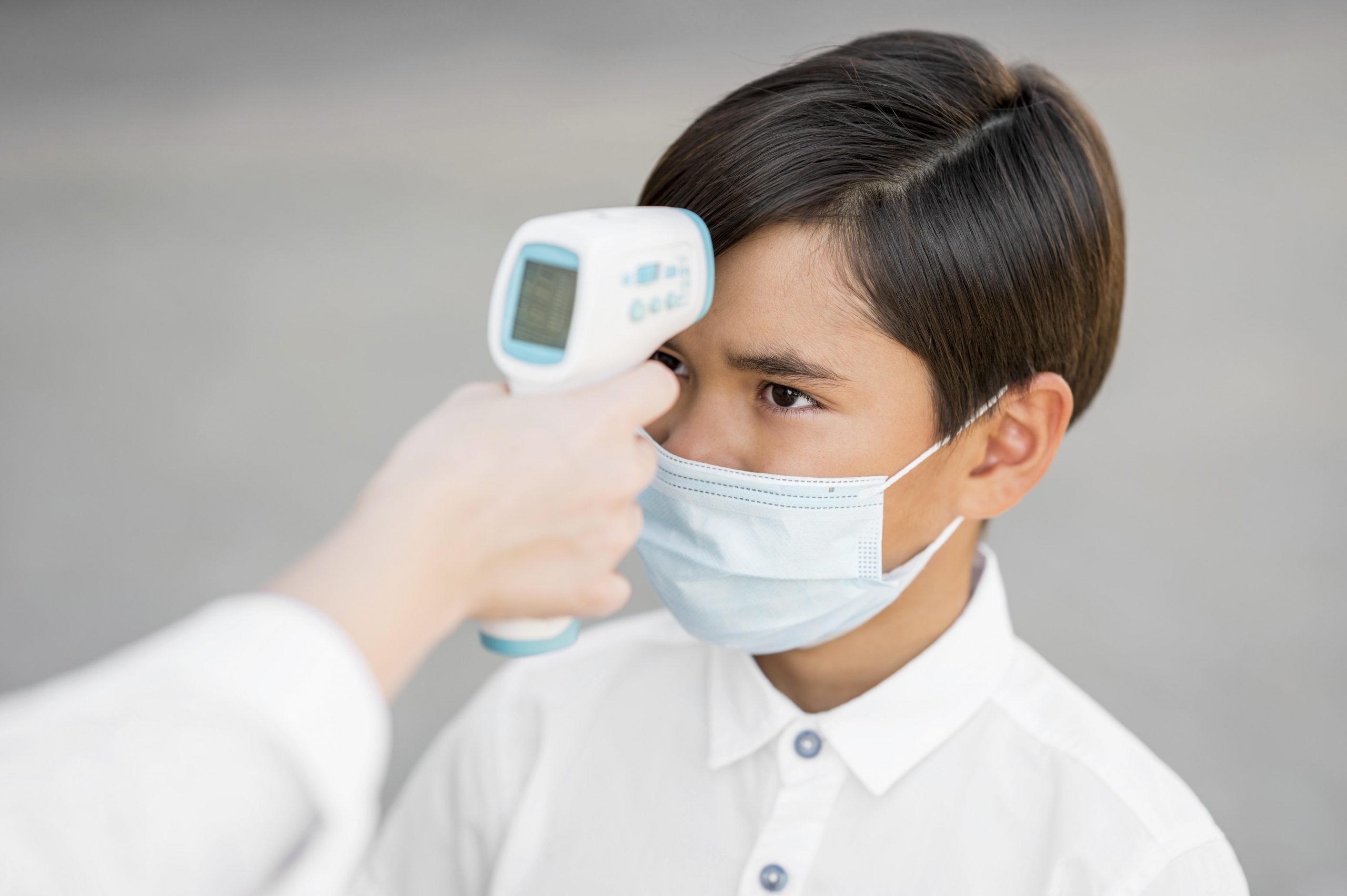
If you’ve ever suspected you had a fever but couldn’t find a thermometer, you’re not alone. The most prevalent symptom of COVID-19 and an early indicator of many other viral diseases is fever. A temperature check can be critical for fast diagnoses and preventing viral spread. Despite the increase in telemedicine consultations, accurate at-home thermometers are still uncommon.
There could be several explanations for this. The gadgets can cost anything from $15 to $300, and many people only use them a few times a year. Thermometers can sell out quickly in times of high demand, such as in the early days of the COVID-19 pandemic. Many people, particularly those in underserved areas, may find themselves without a critical medical device when they require it.
To address this issue, a team led by the University of Washington researchers developed FeverPhone, a software that converts cellphones into thermometers without the addition of new hardware. Instead, it makes use of the phone’s touchscreen and repurposes the existing battery temperature sensors to collect data that is then used by a machine learning algorithm to estimate people’s core body temperatures.
The app measured core body temperatures with accuracy comparable to some consumer thermometers when the researchers tested it on 37 patients in an emergency department. The team’s findings were published on March 28 in the Proceedings of the ACM on Interactive, Mobile, Wearable, and Ubiquitous Technologies.
“In undergrad, I was doing research in a lab where we wanted to show that you could use the temperature sensor in a smartphone to measure air temperature,” said lead author Joseph Breda, a UW doctoral student in the Paul G. Allen School of Computer Science & Engineering. “When I came to the UW, my advisor and I wondered how we could apply a similar technique for health. We decided to measure fever in an accessible way. The primary concern with temperature isn’t that it’s a difficult signal to measure; it’s just that people don’t have thermometers.”
The app is the first to evaluate whether users have fevers using existing phone sensors and screens. Breda believes that additional training data is needed before such technology can be widely employed, but the promise of such technology is exciting for doctors.
“People come to the ER all the time saying, ‘I think I was running a fever.’ And that’s very different than saying ‘I was running a fever,'” said Dr. Mastafa Springston, a co-author on the study and a UW clinical instructor at the Department of Emergency Medicine in the UW School of Medicine. “In a wave of influenza, for instance, people running to the ER can take five days, or even a week sometimes. So if people were to share fever results with public health agencies through the app, similar to how we signed up for COVID exposure warnings, this earlier sign could help us intervene much sooner.
Clinical-grade thermometers use tiny sensors known as thermistors to estimate body temperature. Off-the-shelf smartphones also happen to contain thermistors; they’re mostly used to monitor the temperature of the battery. But the UW researchers realized they could use these sensors to track heat transfer between a person and a phone. The phone touchscreen could sense skin-to-phone contact, and the thermistors could gauge the air temperature and the rise in heat when the phone touched a body. To put this theory to the test, the researchers began by collecting data in a lab. The researchers used a sous-vide machine to heat a plastic bag of water and put phone screens against it to simulate a warm forehead. The researchers evaluated three phone models to account for changes in situations, such as different persons using various phones. They also altered the pressure on the phone and added accessories such as a screen protector and a case.
The researchers collected data from several test cases to construct a machine-learning model that estimated body temperature using complicated interactions.
Because the sensors are designed to measure the temperature of the phone’s battery, the program analyzes how quickly the phone heats up and then utilizes touchscreen data to account for how much of that is due to a person touching it. The researchers were able to adjust the model to account for changes in items like phone accessories as they added additional test cases.
The team was then ready to put the software through its paces on real people. FeverPhone was taken to the UW School of Medicine’s Emergency Department for a clinical trial in which its temperature estimates were compared to an oral thermometer reading. They enlisted the help of 37 people, 16 of whom had at least a slight fever.
The participants used FeverPhone by holding the phones like point-and-shoot cameras, with forefingers and thumbs contacting the corner corners to decrease the heat from the hands being sensed (some had the researcher hold the phone for them). Then, for roughly 90 seconds, participants held the touchscreen on their foreheads, which the researchers discovered was the optimal time to detect body heat flowing to the phone.
FeverPhone evaluated patient core body temperatures with an average inaccuracy of roughly 0.41 degrees Fahrenheit (0.23 degrees Celsius), which is within the clinically acceptable range of 0.5 degrees Celsius. The researchers have identified a few areas for additional research. According to the researchers, participants with severe fevers exceeding 101.5 F (38.6 C) were excluded from the trial because these temperatures are straightforward to diagnose and sweaty skin tends to confound other skin-contact thermometers. Furthermore, FeverPhone was only tested on three phone models. Training it to run on other cellphones as well as gadgets like smartwatches would expand its potential for public health applications, according to the team.
“We started with smartphones since they’re ubiquitous and easy to get data from,” Breda said. “I am already working on seeing if we can get a similar signal with a smartwatch. What’s nice, because watches are much smaller, is their temperature will change more quickly. So you could imagine having a user put a Fitbit to their forehead and measure in 10 seconds whether they have a fever or not.”
Shwetak Patel, a UW professor in the Allen School and the electrical and computer engineering department, was a senior author of the paper, and Alex Mariakakis, an assistant professor in the University of Toronto’s computer science department, was a co-author.
more recommended stories
 Fragmentome Technology Detects Early Liver Fibrosis
Fragmentome Technology Detects Early Liver FibrosisKey Points at a Glance AI-based.
 AI Predicts Chronic GVHD Risk After Stem Cell Transplant
AI Predicts Chronic GVHD Risk After Stem Cell TransplantKey Takeaways A new AI-driven tool,.
 Rising Measles Cases Prompt Vaccination Push in NC
Rising Measles Cases Prompt Vaccination Push in NCKey Highlights 15 confirmed Measles cases.
 High-Fat Diets Cause Damage to Metabolic Health
High-Fat Diets Cause Damage to Metabolic HealthKey Points Takeaways High-fat and ketogenic.
 Chronic Brain Compression Triggers Neuron Death Pathways
Chronic Brain Compression Triggers Neuron Death PathwaysKey Takeaways Chronic brain compression directly.
 Texas Medical Board Releases Abortion Training for Physicians
Texas Medical Board Releases Abortion Training for PhysiciansKey Takeaways Texas Medical Board has.
 Needle-Thin Brain Implant for Layer-Specific Brain Research
Needle-Thin Brain Implant for Layer-Specific Brain ResearchKey Takeaways Researchers have developed a.
 Pancreatic Cancer Research: Triple-Drug Therapy Success
Pancreatic Cancer Research: Triple-Drug Therapy SuccessKey Summary Spanish researchers report complete.
 Immune Cell Epigenome Links Genetics and Life Experience
Immune Cell Epigenome Links Genetics and Life ExperienceKey Takeaway Summary Immune cell responses.
 Chronic Pain Linked to CGIC Brain Circuit, Study Finds
Chronic Pain Linked to CGIC Brain Circuit, Study FindsKey Takeaways University of Colorado Boulder.

Leave a Comment