The loss of a gene called SYNCRIP in prostate cancer tumors activates cellular machinery that causes random mutations throughout the genome, leading to resistance to targeted treatments, according to a team led by UT Southwestern Medical Center researchers. The results, which were published in Cancer Cell, could lead to new therapies that disrupt this process in prostate and other cancer types, making them significantly more treatable.
“This study paves the way for innovative strategies to fix the broken ‘brake’ for mutagenesis in cancer and curb resistance to treatments,” said study leader Ping Mu, Ph.D., Assistant Professor of Molecular Biology at UT Southwestern and a member of the Harold C. Simmons Comprehensive Cancer Center.
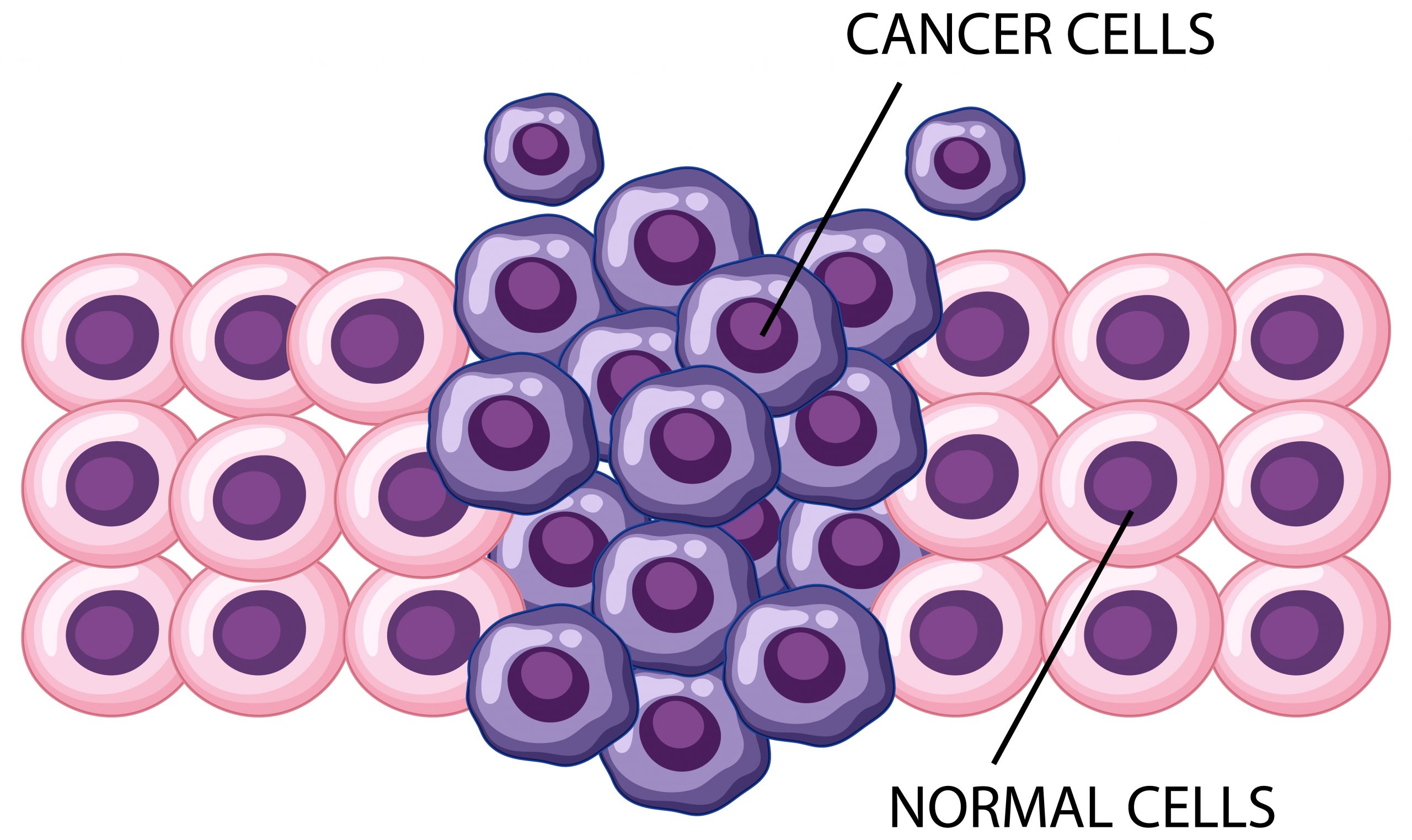
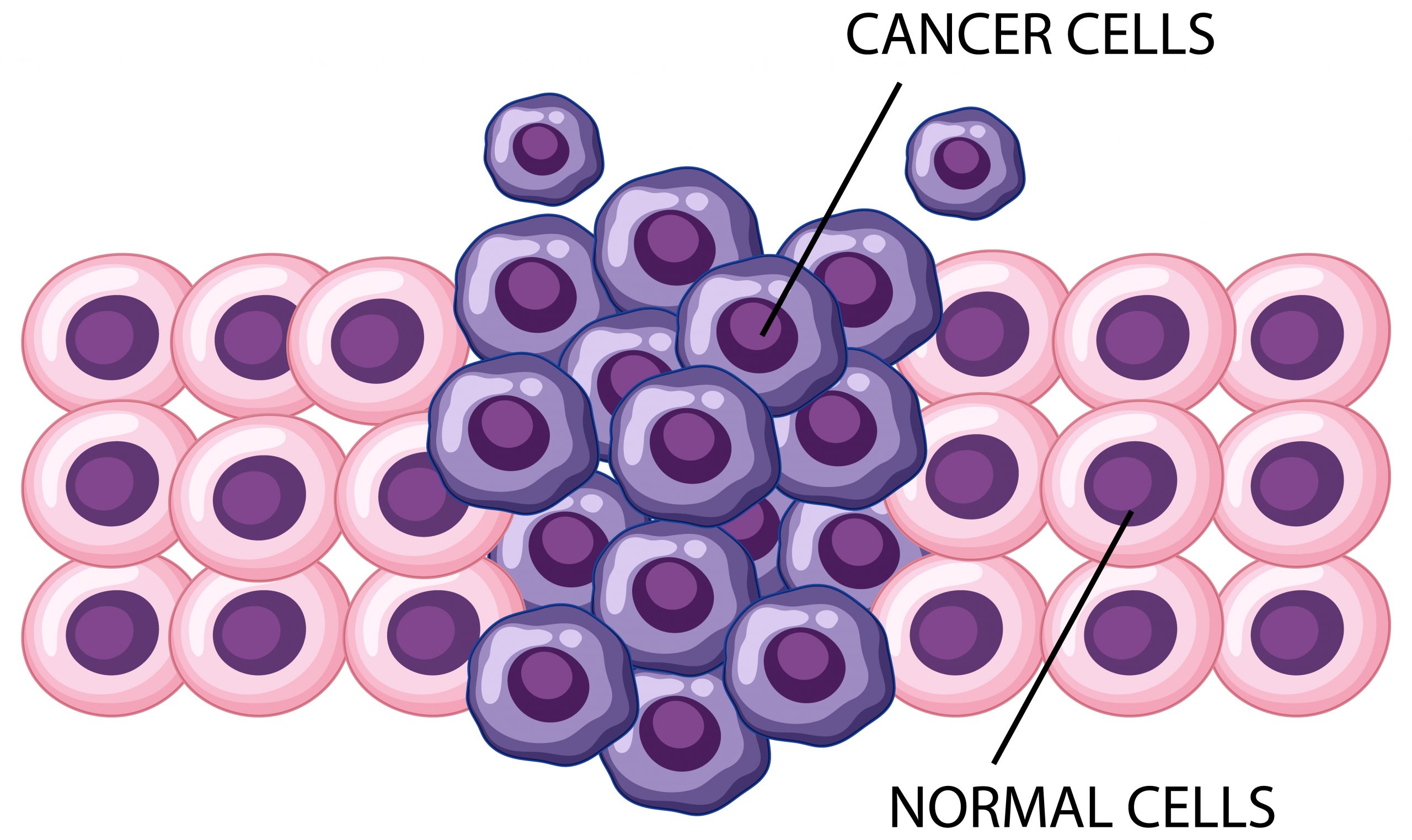
Researchers have long known that many cancers are caused by DNA abnormalities, and that more mutations regularly arise, causing tumors to grow and spread. Although medications exist to target tumors with specific mutations, they do not address the entire spectrum of alterations that occur in cancer cells, according to Dr. Mu. As a result, the more mutations a tumor has, the more resistant it is to treatment. However, it is unknown how and why these extra mutations occur so quickly.
Dr. Mu and his colleagues sought genetic differences in the cells of prostate cancer tumors – the Mu lab’s focus – from samples taken from xenografted human tumors before and after antiandrogen therapy, a common treatment that deprives prostate cancers of sex hormones that can fuel their growth. Although this treatment is frequently effective at first, prostate cancers almost always develop resistance to antiandrogen therapy with time.
The SYNCRIP gene had vanished in almost half of the post-treatment samples. The researchers also discovered a number of mutations that bore the signature of APOBEC proteins, which are pieces of cellular machinery that produce a specific form of mutation used for immunological protection in healthy cells.
Further research suggests that SYNCRIP acts as a brake for APOBEC3B, a prominent member of the APOBEC protein family, keeping its activity under check. Dr. Mu noted that when SYNCRIP is lost, APOBEC3B’s function becomes unregulated, resulting in random mutations throughout the genome. Even in the absence of SYNCRIP, cells genetically engineered to eliminate APOBEC3B did not develop mutations, suggesting that their roles are connected.
The researchers analyzed the genomes of post-treatment cells for APOBEC-induced mutations that caused genes to become hyperactive in search of genetic drivers of treatment resistance that originate from this process. They discovered eight genes that appear to be hotspots for APOBEC-driven mutations, and all of them rendered antiandrogen therapy ineffective. The cells became sensitive to therapy again when the researchers removed these genes from them.
Because APOBEC hallmark mutations are prevalent in over 70% of human tumors, the findings shed light on various oncology puzzles, according to Dr. Mu. These include why carcinogenic tumors tend to develop so many mutations so quickly and why the mutation pattern varies between people with the same cancer type and, in some cases, between cells in the same tumor.
Currently, tumors are treated by treating these mutations individually, which is successful only if a targeted treatment for a specific mutation exists, he added. Researchers may be able to design medicines that restore SYNCRIP or suppress APOBEC proteins in the future to prevent resistance-driving mutations from developing.
more recommended stories
 AI Predicts Chronic GVHD Risk After Stem Cell Transplant
AI Predicts Chronic GVHD Risk After Stem Cell TransplantKey Takeaways A new AI-driven tool,.
 Red Meat Consumption Linked to Higher Diabetes Odds
Red Meat Consumption Linked to Higher Diabetes OddsKey Takeaways Higher intake of total,.
 Pediatric Crohn’s Disease Microbial Signature Identified
Pediatric Crohn’s Disease Microbial Signature IdentifiedKey Points at a Glance NYU.
 Nanovaccine Design Boosts Immune Attack on HPV Tumors
Nanovaccine Design Boosts Immune Attack on HPV TumorsKey Highlights Reconfiguring peptide orientation significantly.
 High-Fat Diets Cause Damage to Metabolic Health
High-Fat Diets Cause Damage to Metabolic HealthKey Points Takeaways High-fat and ketogenic.
 Acute Ischemic Stroke: New Evidence for Neuroprotection
Acute Ischemic Stroke: New Evidence for NeuroprotectionKey Highlights A Phase III clinical.
 Statins Rarely Cause Side Effects, Large Trials Show
Statins Rarely Cause Side Effects, Large Trials ShowKey Points at a Glance Large.
 Anxiety Reduction and Emotional Support on Social Media
Anxiety Reduction and Emotional Support on Social MediaKey Summary Anxiety commonly begins in.
 Liquid Biopsy Measures Epigenetic Instability in Cancer
Liquid Biopsy Measures Epigenetic Instability in CancerKey Takeaways Johns Hopkins researchers developed.
 Human Antibody Drug Response Prediction Gets an Upgrade
Human Antibody Drug Response Prediction Gets an UpgradeKey Takeaways A new humanized antibody.

Leave a Comment