CRISPR, the gene-editing technique that has transformed biological research, is now available as a medical treatment that has received regulatory approval. The first CRISPR treatment for sickle cell disease was authorized by the US Food and Drug Administration on December 8.
The exa-cel therapy, developed by Vertex and CRISPR Therapeutics, modifies a gene involved in red blood cell shape and function. It appears to be effective in curing the condition for at least a year. Following the approval of exa-cel for sickle cell disease in the United Kingdom in November, the FDA’s decision makes the United States the second country to authorize a CRISPR medicine.
Exa-cel is “an incredible asset to have,” according to Michael DeBaun, a hematologist at Vanderbilt University. However, it is too early to tell if the treatment will be lasting and free of adverse effects, he says.
The FDA also approved lovo-cel, a sort of gene therapy for sickle cell disease developed by the company bluebird bio, today.
HOW DOES THE NEW CRISPR THERAPY WORK FOR SICKLE CELL DISEASE?
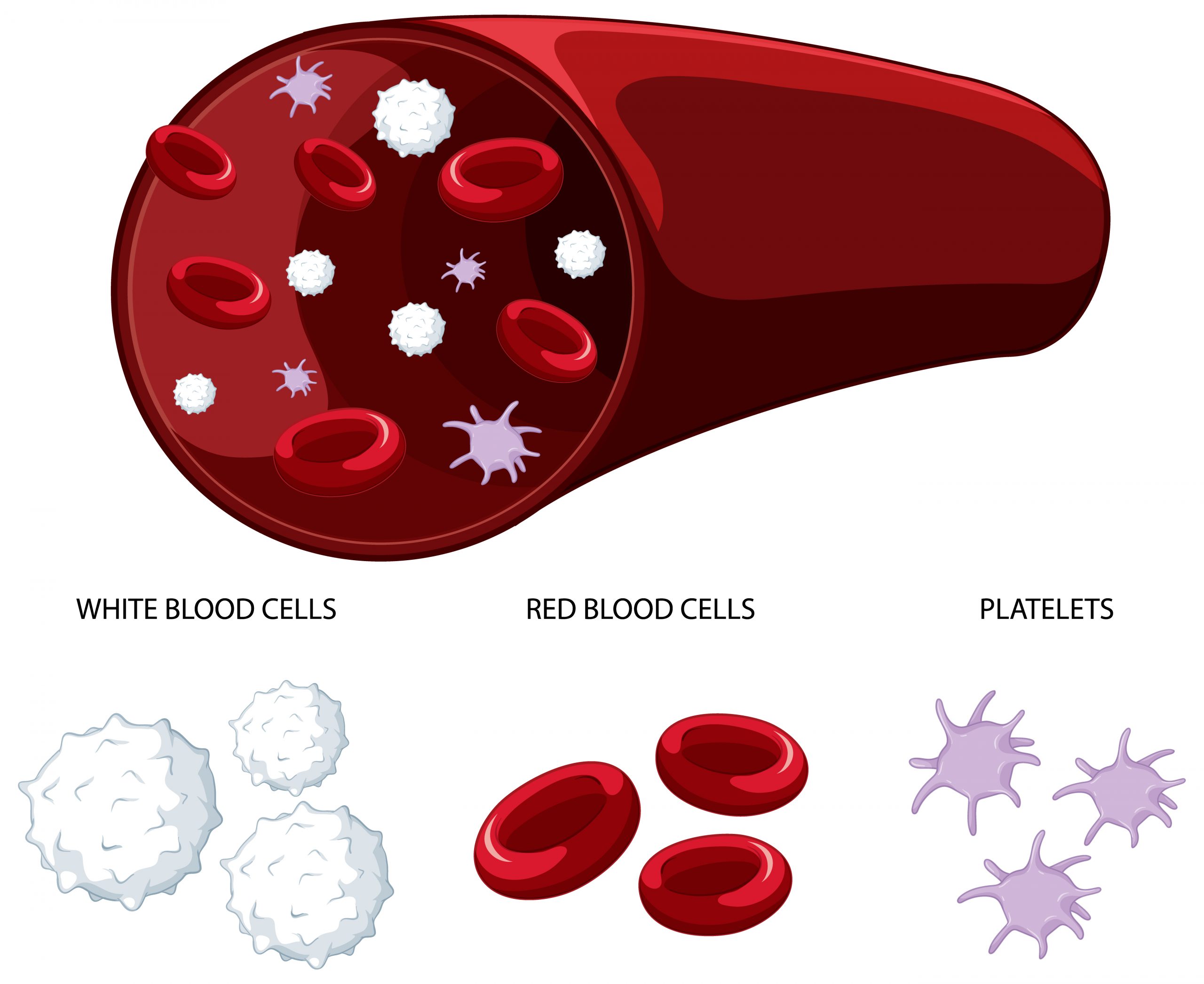
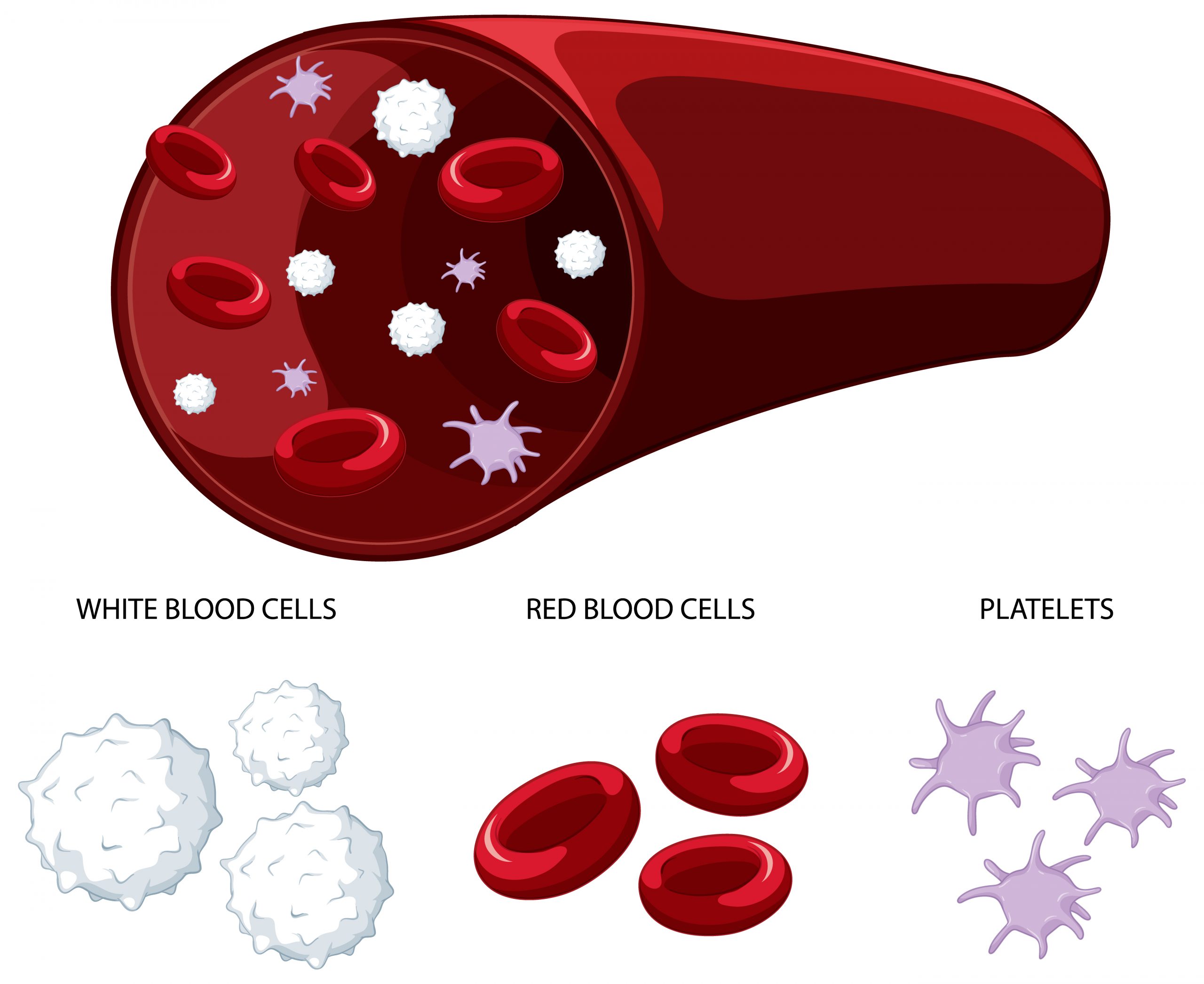
The exa-cel CRISPR system targets genes that create hemoglobin, the molecule that transports oxygen in blood cells. Mutations in a gene called HBB disrupt the structure of the protein, leading it to twist normally round red blood cells into a curved sickle shape in sickle cell anemia. These sickled cells choke blood vessels, causing excruciating agony and weariness. In beta-thalassemia, a disorder related to sickle cell anemia, the body does not create enough hemoglobin or red blood cells, resulting in symptoms caused by low blood oxygen levels. In children, these symptoms include weariness and development issues.
Exa-cel leads the Cas9 enzyme to a gene called BCL11A, which normally inhibits the body from producing a kind of hemoglobin seen only in fetuses. Cas9 deactivates BCL11A in bone marrow stem cells, where red blood cells are formed, by breaking its DNA, and the cells begin generating fetal hemoglobin and forming typical round red blood cells. The novel therapy involves removing a person’s own bone marrow stem cells, editing them with exa-cel, destroying the remainder of the person’s untreated bone marrow, and reinfusing the edited cells.
Because these modified cells eventually repopulate the body, exa-cel is termed a “curative” therapy that will theoretically last the recipient’s entire life, despite the fact that Vertex and CRISPR Therapeutics have only monitored the majority of their trial participants for less than two years.
WHAT IS THE EFFECTIVENESS OF THE TREATMENT?
Exa-cel has only been tried on about 100 persons with sickle cell anemia or beta-thalassemia thus far. Nonetheless, the FDA granted the businesses “fast-track” approval in 2019, allowing them to test the therapy in smaller groups of individuals than would otherwise be required.
In these continuing trials, 29 of the 30 research participants with sickle cell anemia reported no pain for one year after receiving exa-cel infusions. And, one year after the exa-cel intervention, 39 of 42 beta-thalassemia patients no longer required blood or bone marrow transplants, the conventional treatment for this disease. Vertex and CRISPR Therapeutics are continuing to study the remaining participants who have not yet reached this time point and will do so for up to 15 years.
WHAT ARE THE DANGERS?
According to the data given to the FDA, exa-cel has no significant negative health consequences, albeit it can produce nausea and fever. However, DeBaun points out that the participants have only been tracked for a short period of time, and difficulties may occur later.
The FDA also expressed worry that the Cas9 enzyme could remain active and cut the DNA in places other than BCL11A, resulting in so-called off-target alterations. The firms modeled the most likely sites in the genome where the enzyme could cut and discovered no evidence of this occurring in trial participants. “In light of any new therapy, we remain cautiously optimistic,” she says.
WHAT OTHER PROMISING THERAPIES FOR SICKLE CELL DISEASE ARE THERE APART FROM EXA-CEL?
The other gene therapy approved by the FDA today is Bluebird bio’s lovo-cel, which employs a viral vector to deliver a functional form of an adult hemoglobin-producing gene and permanently insert it into a person’s DNA. According to the data provided to the FDA by Bluebird Bio, lovo-cel was effective in 36 persons who were monitored for a median of 32 months. Several trials are currently being conducted to investigate various types of gene treatments for sickle cell anemia and beta-thalassemia that transfer normal versions of HBB or other genes to the body.
A procedure known as haploidentical transplant has been discovered to cure sickle cell anemia. A person’s bone marrow cells are replaced with those from a parent or sibling who is 50 percent genetically identical to the receiver but does not have the disease in this treatment, which is already commonly used to treat some cancers. According to findings that will be presented next week at the annual conference of the American Society for Hematology, 88 percent of persons who got these transplants continued to produce normal red blood cells after two years. According to DeBaun, this method could be especially valuable in low- and middle-income nations because it is anticipated to be significantly less expensive than gene editing or gene therapy.
WILL EVERYONE WITH SICKLE CELL DISEASE BE ABLE TO ACCESS EXA-CEL OR LOVO-CELL?
Exa-cel and lovo-cell, like most gene editing medicines, are expected to be prohibitively expensive. Vertex, CRISPR Therapeutics, and Bluebird Bio have not disclosed the price of their various medicines, although estimates imply that each might cost up to $2 million per patient. It is still unknown if insurers, particularly government-funded programs like Medicaid, would cover the medicines or in which situations they will. Sickle cell illness disproportionately affects people of African origin, including African Americans, who are more likely than most other groups in the United States to have public insurance through Medicaid.
According to DeBaun, the decision to seek CRISPR gene editing or another option, such as haploidentical transplant, will need to be made collaboratively by patients, their families, and their physicians. Even if gene editing is more effective at permanently curing the disease, it will be less readily available and may take longer than a donor transplant.
Nonetheless, DeBaun believes that exa-cel is a promising starting step and that the technology will improve as more about CRISPR medicines is discovered over the next decade. “This is the first mile of a marathon,” he said.
more recommended stories
 Nanoplastics in Brain Tissue and Neurological Risk
Nanoplastics in Brain Tissue and Neurological RiskKey Takeaways for HCPs Nanoplastics are.
 AI Predicts Chronic GVHD Risk After Stem Cell Transplant
AI Predicts Chronic GVHD Risk After Stem Cell TransplantKey Takeaways A new AI-driven tool,.
 Red Meat Consumption Linked to Higher Diabetes Odds
Red Meat Consumption Linked to Higher Diabetes OddsKey Takeaways Higher intake of total,.
 Pediatric Crohn’s Disease Microbial Signature Identified
Pediatric Crohn’s Disease Microbial Signature IdentifiedKey Points at a Glance NYU.
 Nanovaccine Design Boosts Immune Attack on HPV Tumors
Nanovaccine Design Boosts Immune Attack on HPV TumorsKey Highlights Reconfiguring peptide orientation significantly.
 High-Fat Diets Cause Damage to Metabolic Health
High-Fat Diets Cause Damage to Metabolic HealthKey Points Takeaways High-fat and ketogenic.
 Acute Ischemic Stroke: New Evidence for Neuroprotection
Acute Ischemic Stroke: New Evidence for NeuroprotectionKey Highlights A Phase III clinical.
 Statins Rarely Cause Side Effects, Large Trials Show
Statins Rarely Cause Side Effects, Large Trials ShowKey Points at a Glance Large.
 Anxiety Reduction and Emotional Support on Social Media
Anxiety Reduction and Emotional Support on Social MediaKey Summary Anxiety commonly begins in.
 Liquid Biopsy Measures Epigenetic Instability in Cancer
Liquid Biopsy Measures Epigenetic Instability in CancerKey Takeaways Johns Hopkins researchers developed.

Leave a Comment