Hip replacement surgery is safe for HIV patients, according to researchers at the University of Texas Southwestern Medical Center.
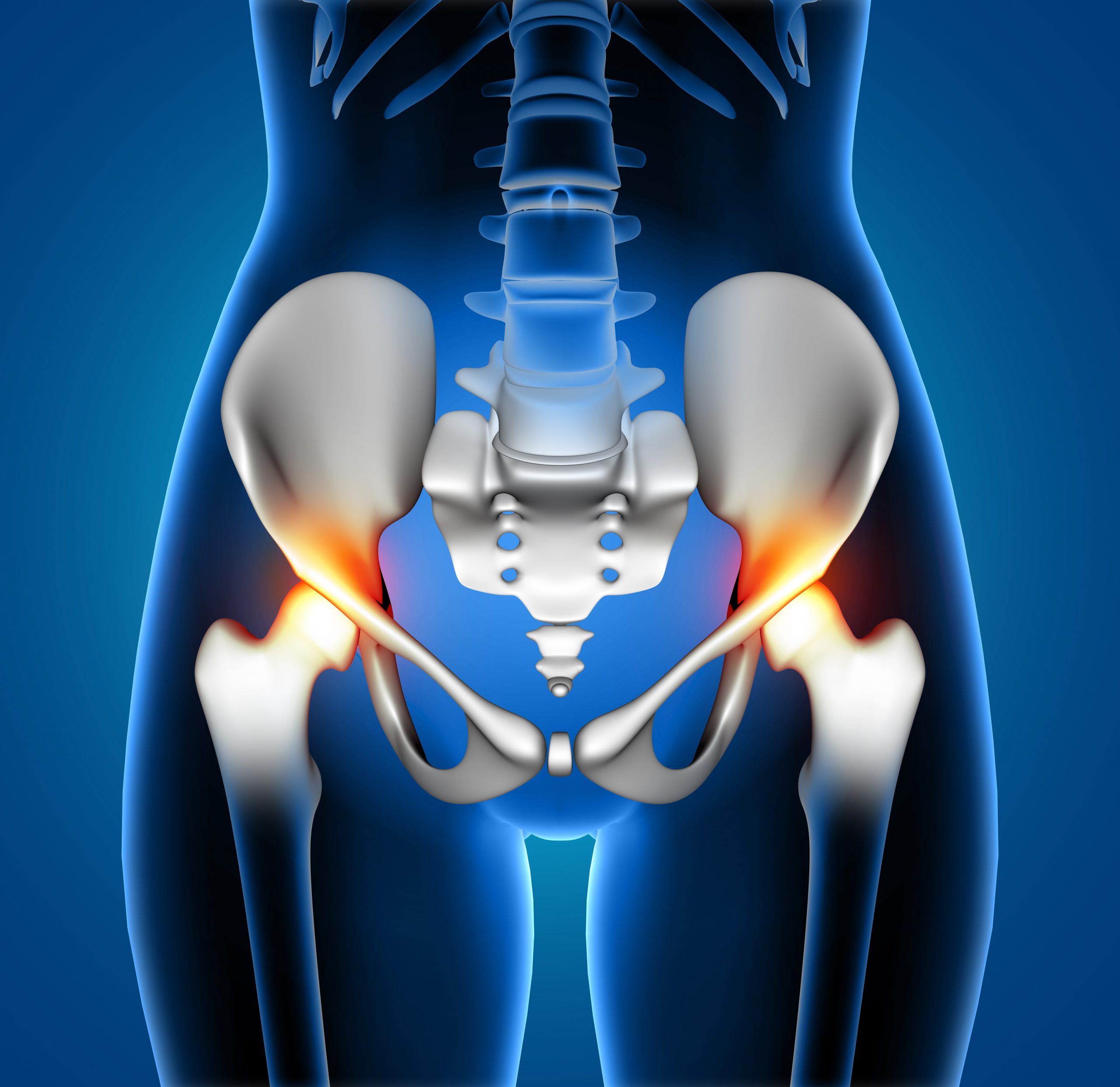
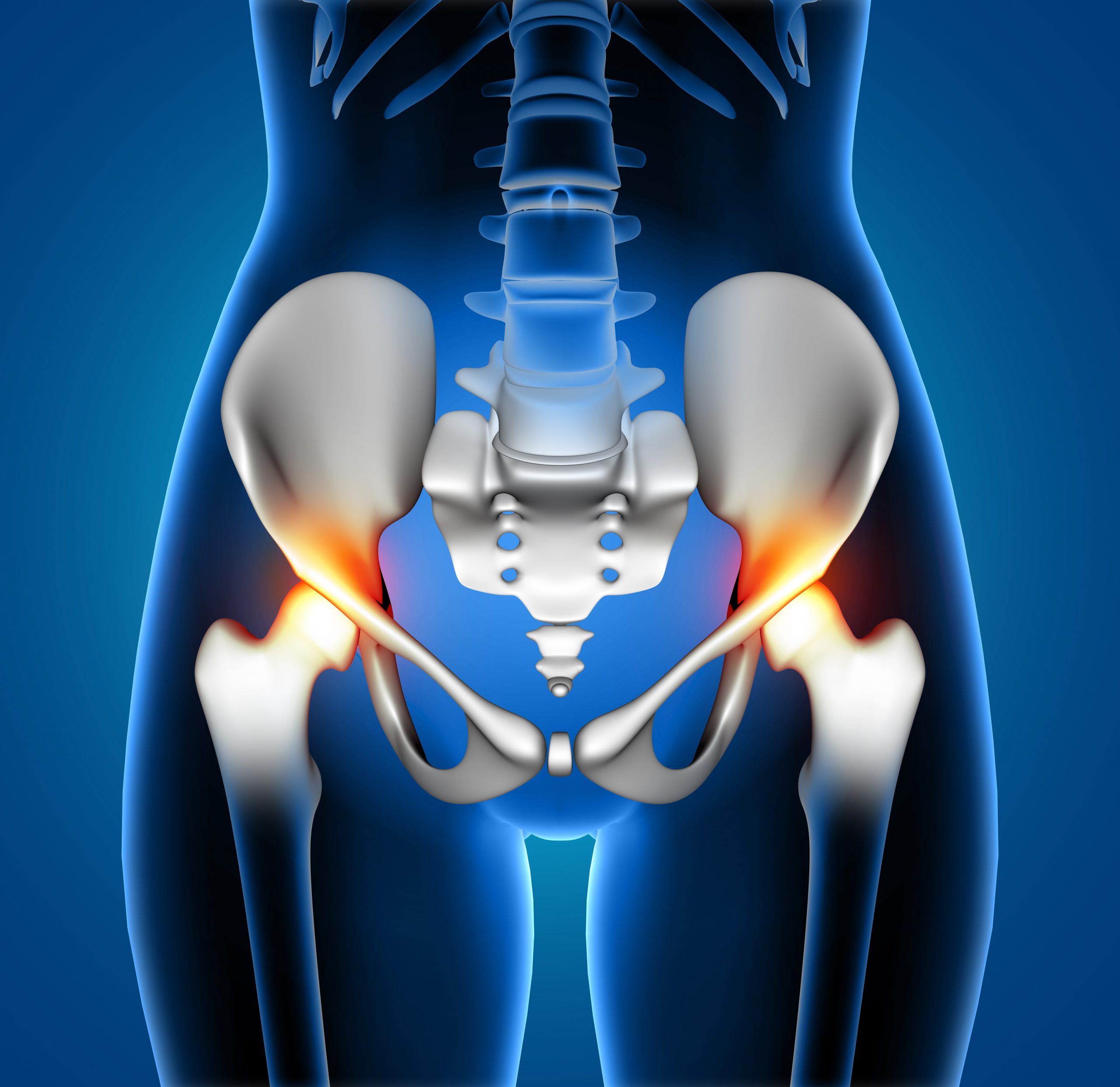
Total hip arthroplasty (THA) is a frequent treatment performed largely on elderly patients with osteoarthritis or osteonecrosis, both of which are painful disorders that significantly limit mobility and lifestyle options. However, some surgeons have been cautious to perform THAs on HIV/AIDS patients due to worries about complications, such as an increased risk of infection, the need for revision surgery, and an extended hospital stay.
“Patients living with HIV are at a higher risk for orthopedic-related diseases such as osteoarthritis or osteonecrosis of the hip due to changes in their bone metabolism and effects from their medication regimen,” said Senthil Sambandam, M.D., Assistant Professor of Orthopaedic Surgery, who led the study. “With improvements in HIV treatment leading to increased life expectancies, we are seeing a rise in the need for THA procedures in this patient population. Our study demonstrates that HIV-positive patients can safely undergo THA without concern for increased risk of complications and adds to the growing amount of literature that encourages surgeons to deliver appropriate medical care to a marginalized patient population.”
UTSW researchers identified 504 HIV-positive patients who underwent THAs using data from the National Inpatient Sample from 2016 to 2019 and compared their postoperative problems to a group of 493 HIV-negative individuals. Postoperative complications such as pneumonia, periprosthetic infection, wound dehiscence (reopening), and superficial and deep surgical site infection were not significantly different between the HIV-positive and negative groups, according to their findings published in the Journal of Clinical Orthopaedics and Trauma. Blood transfusion rates were similarly lower in HIV-positive individuals.
The research was part of a larger effort by the Department of Orthopaedic Surgery to examine arthroplasty problems in various subpopulations in order to support UTSW’s commitment to the care of underserved patient populations and equal treatment for all patients.
“These are important findings because they can help alleviate worries among the medical community about treating a group of patients who are often overlooked,” Dr. Sambandam said. “It’s an important quality-of-life issue for many HIV-positive patients.”
more recommended stories
 AI Predicts Chronic GVHD Risk After Stem Cell Transplant
AI Predicts Chronic GVHD Risk After Stem Cell TransplantKey Takeaways A new AI-driven tool,.
 Red Meat Consumption Linked to Higher Diabetes Odds
Red Meat Consumption Linked to Higher Diabetes OddsKey Takeaways Higher intake of total,.
 Pediatric Crohn’s Disease Microbial Signature Identified
Pediatric Crohn’s Disease Microbial Signature IdentifiedKey Points at a Glance NYU.
 Nanovaccine Design Boosts Immune Attack on HPV Tumors
Nanovaccine Design Boosts Immune Attack on HPV TumorsKey Highlights Reconfiguring peptide orientation significantly.
 High-Fat Diets Cause Damage to Metabolic Health
High-Fat Diets Cause Damage to Metabolic HealthKey Points Takeaways High-fat and ketogenic.
 Acute Ischemic Stroke: New Evidence for Neuroprotection
Acute Ischemic Stroke: New Evidence for NeuroprotectionKey Highlights A Phase III clinical.
 Statins Rarely Cause Side Effects, Large Trials Show
Statins Rarely Cause Side Effects, Large Trials ShowKey Points at a Glance Large.
 Anxiety Reduction and Emotional Support on Social Media
Anxiety Reduction and Emotional Support on Social MediaKey Summary Anxiety commonly begins in.
 Liquid Biopsy Measures Epigenetic Instability in Cancer
Liquid Biopsy Measures Epigenetic Instability in CancerKey Takeaways Johns Hopkins researchers developed.
 Human Antibody Drug Response Prediction Gets an Upgrade
Human Antibody Drug Response Prediction Gets an UpgradeKey Takeaways A new humanized antibody.

Leave a Comment