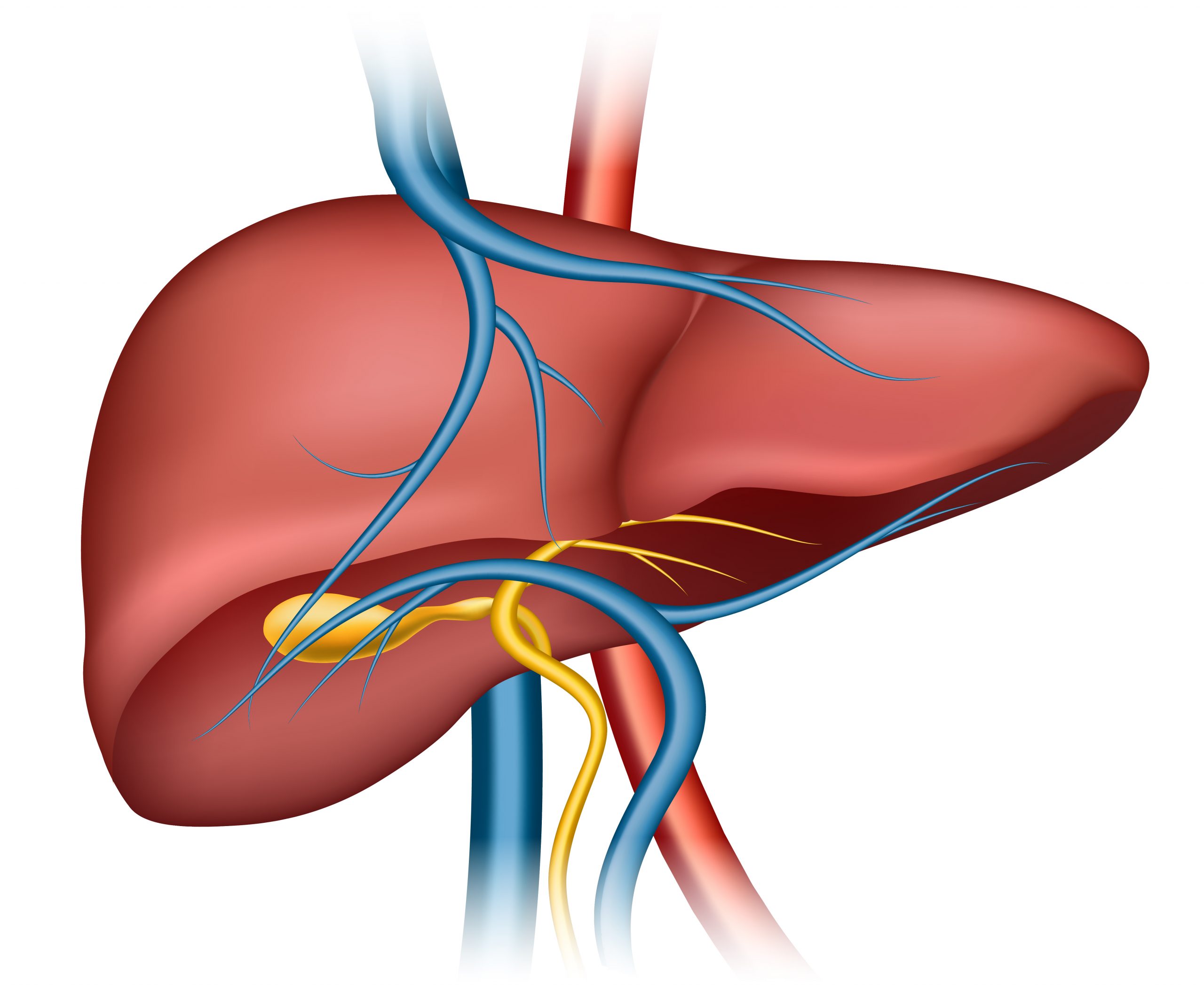
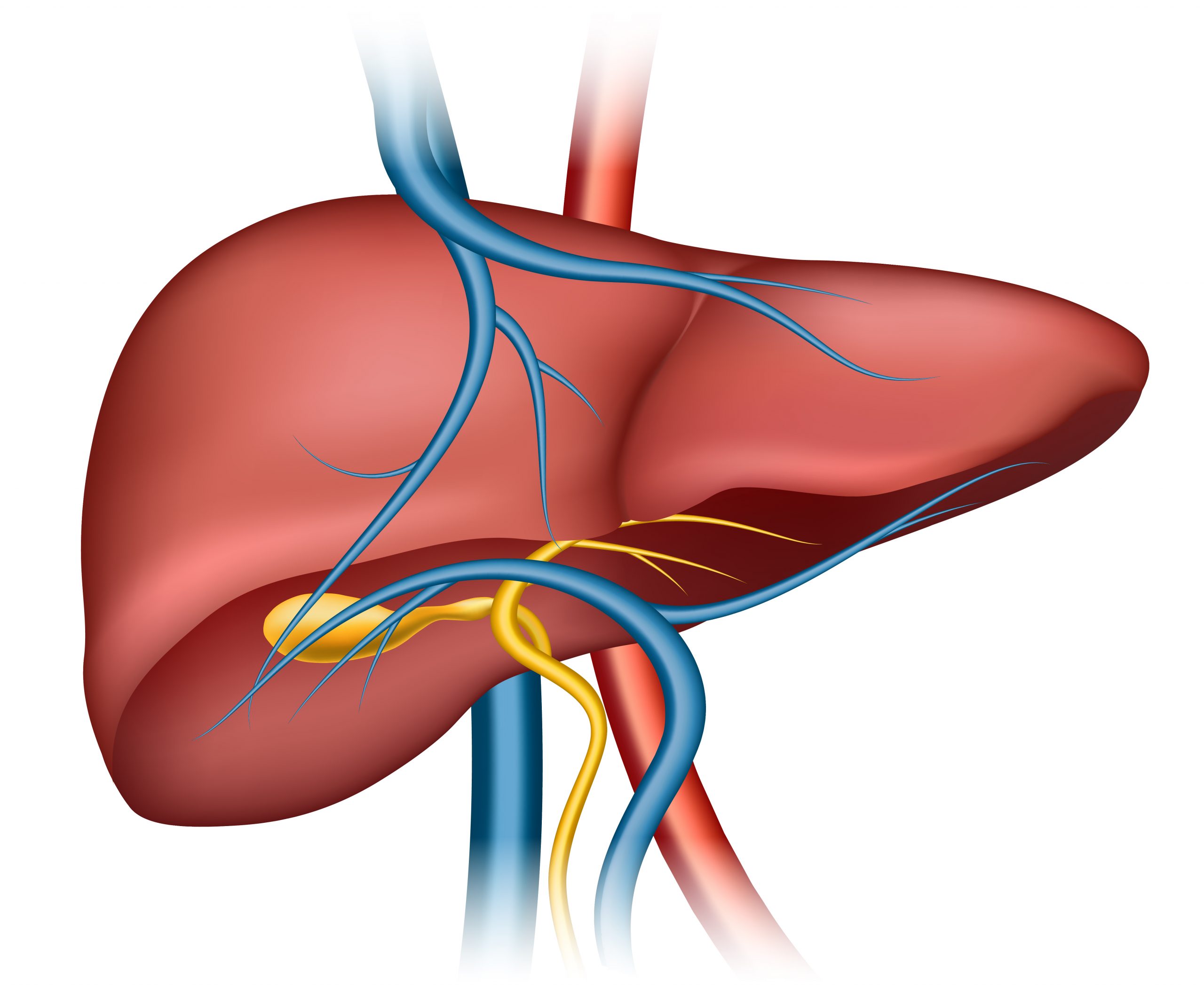
A study led by researchers at the University of California San Diego School of Medicine looked into a possible new therapy option for patients with liver disease called non-alcoholic steatohepatitis (NASH)-related fibrosis.
The findings, published in the online edition of The New England Journal of Medicine on June 24, 2023, discovered that a medicine that mimics a hormone in the body decreased both liver fibrosis and liver inflammation in NASH patients.
“Identifying an effective drug for NASH is extremely promising for patients as currently there are no FDA-approved therapies for this condition,” said Rohit Loomba, MD, the study’s first author and chief of the Division of Gastroenterology and Hepatology at UC San Diego School of Medicine. “NASH can adversely impact the quality of life in patients and can progress to cirrhosis. Its complications can lead to death or liver transplantation. Our findings will further the science of this disease and provide a potential new treatment option to those affected by NASH-related fibrosis.”
The researchers discovered that the medicine, termed pegozafermin, mimicked fibroblast growth factor 21 (FGF21), a naturally occurring peptide hormone generated by the liver.
FGF21 regulates energy metabolism in the organism as well as lipid metabolism in the liver. Previous research has also demonstrated that it lowers blood glucose and insulin levels, as well as body weight and liver fat.
“The study’s results show that the new potential treatment not only improves fibrosis but also improves inflammation and liver injury along with significant improvements across multiple non-invasive biomarkers of NASH activity and scarring,” said Loomba, gastroenterologist and hepatologist at UC San Diego Health.
The 24-week randomized clinical trial included 222 NASH patients who were randomly assigned to either the medication or a placebo. Approximately 27% of patients who received the medicine at a higher dose improved in liver fibrosis, compared to 7% of patients who received the placebo. The drug’s most often reported side effects were gastrointestinal in nature, including nausea.
There are currently no drugs approved by the US Food and Drug Administration for the treatment of NASH, a type of nonalcoholic fatty liver disease (NAFLD).
According to the National Institutes of Health, around 24% of adults in the United States have NAFLD, and roughly 6% have NASH.
NAFLD and NASH are considered silent diseases since they have few to no symptoms; nevertheless, people who are overweight, have type 2 diabetes, or have a family member with NAFLD are more likely to develop the disease. NAFLD, an umbrella term for a variety of liver problems affecting people who use little to no alcohol, can result in cirrhosis, liver cancer, and liver failure.
The next phase in this research, according to Loomba, will be a larger, multi-center, multinational trial with a more diversified patient group and a longer treatment time to properly examine the drug’s safety.
If successfully shown to be both safe and effective in a larger Phase 3 trial, this drug could be used to treat millions of patients with NASH, including our patients at UC San Diego Health,” said Loomba.
more recommended stories
 Red Blood Cells Improve Glucose Tolerance Under Hypoxia
Red Blood Cells Improve Glucose Tolerance Under HypoxiaKey Takeaways for Clinicians Chronic hypoxia.
 Nanoplastics in Brain Tissue and Neurological Risk
Nanoplastics in Brain Tissue and Neurological RiskKey Takeaways for HCPs Nanoplastics are.
 AI Predicts Chronic GVHD Risk After Stem Cell Transplant
AI Predicts Chronic GVHD Risk After Stem Cell TransplantKey Takeaways A new AI-driven tool,.
 Red Meat Consumption Linked to Higher Diabetes Odds
Red Meat Consumption Linked to Higher Diabetes OddsKey Takeaways Higher intake of total,.
 Pediatric Crohn’s Disease Microbial Signature Identified
Pediatric Crohn’s Disease Microbial Signature IdentifiedKey Points at a Glance NYU.
 Nanovaccine Design Boosts Immune Attack on HPV Tumors
Nanovaccine Design Boosts Immune Attack on HPV TumorsKey Highlights Reconfiguring peptide orientation significantly.
 High-Fat Diets Cause Damage to Metabolic Health
High-Fat Diets Cause Damage to Metabolic HealthKey Points Takeaways High-fat and ketogenic.
 Acute Ischemic Stroke: New Evidence for Neuroprotection
Acute Ischemic Stroke: New Evidence for NeuroprotectionKey Highlights A Phase III clinical.
 Statins Rarely Cause Side Effects, Large Trials Show
Statins Rarely Cause Side Effects, Large Trials ShowKey Points at a Glance Large.
 Anxiety Reduction and Emotional Support on Social Media
Anxiety Reduction and Emotional Support on Social MediaKey Summary Anxiety commonly begins in.

Leave a Comment