The healthy human brain contains tens of billions of neurons—specialized cells that process and transmit information via electrical and chemical signals. They send messages between different parts of the brain, and from the brain to the muscles and organs of the body. Alzheimer’s disease disrupts this communication among neurons, resulting in loss of function and cell death.
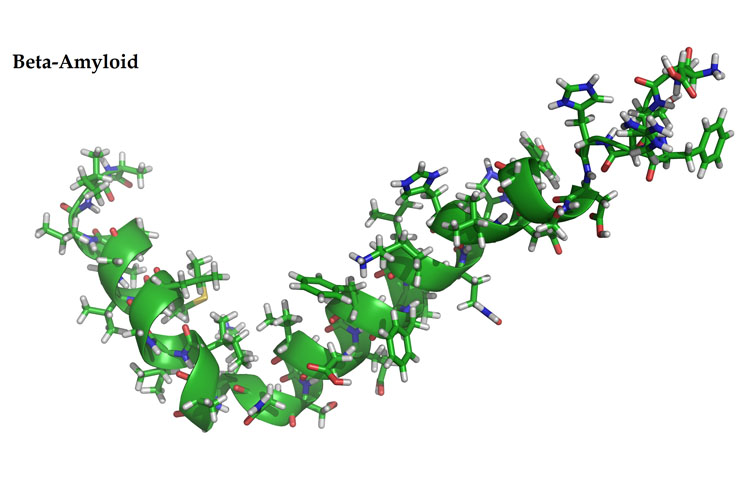
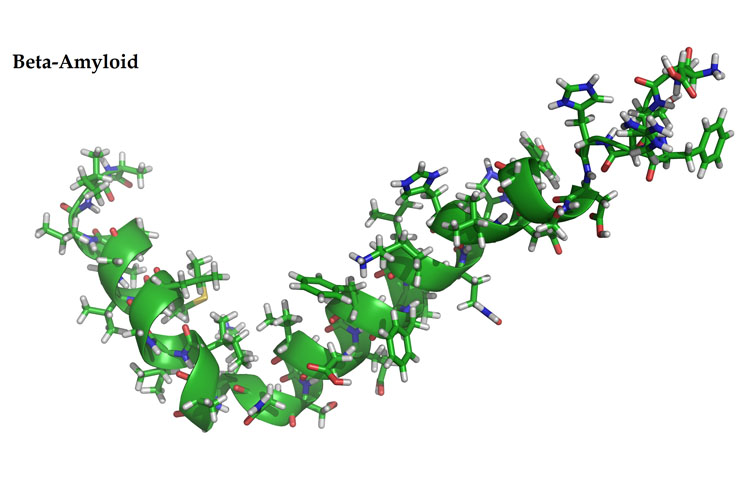
It is formed from the breakdown of a larger protein, called amyloid precursor protein. One form, beta-amyloid 42, is thought to be especially toxic. In the Alzheimer’s brain, abnormal levels of this naturally occurring protein clump together to form plaques that collect between neurons and disrupt cell function.
Recent Study
Newly published research has revealed a close link between proteins associated with Alzheimer’s disease and age-related sight loss. The findings could open the way to new treatments for patients with deteriorating vision and through this study, the scientists believe they could reduce the need for using animals in future research into blinding conditions.
Amyloid beta (Ab) proteins are the primary driver of Alzheimer’s disease but also begin to collect in the retina as people get older. Donor eyes from patients who suffered from age-related macular degeneration (AMD), the most common cause of blindness amongst adults in the UK, have been shown to contain high levels of Ab in their retinas. This new study, published in the journal Cells, builds on previous research which shows that Ab collects around a cell layer called the retinal pigment epithelium (RPE), to establish what damage these toxic proteins cause RPE cells.
The research team exposed RPE cells of normal mouse eyes and in culture to Ab. The mouse model enabled the team to look at the effect the protein has in living eye tissue, using non-invasive imaging techniques that are used in ophthalmology clinics. Their findings showed that the mouse eyes developed retinal pathology that was strikingly similar to AMD in humans.
Dr Arjuna Ratnayaka, a Lecturer in Vision Sciences at the University of Southampton, who led the study said, “This was an important study which also showed that mouse numbers used for experiments of this kind can be significantly reduced in the future.
We were able to develop a robust model to study AMD-like retinal pathology driven by Ab without using transgenic animals, which are often used by researchers the field.
Transgenic or genetically engineered mice can take up to a year and typically longer, before Ab causes pathology in the retina, which we can achieve within two weeks. This reduces the need to develop more transgenic models and improves animal welfare.”
The investigators also used the cell models, which further reduced the use of mice in these experiments, to show that the toxic Ab proteins entered RPE cells and rapidly collected in lysosomes, the waste disposal system for the cells. Whilst the cells performed their usual function of increasing enzymes within lysosomes to breakdown this unwanted cargo, the study found that around 85% of Ab still remained within lysosomes, meaning that over time the toxic molecules would continue to accumulate inside RPE cells.
Furthermore, the researchers discovered that once lysosomes had been invaded by Ab, around 20 percent fewer lysosomes were available to breakdown photoreceptor outer segments, a role they routinely perform as part of the daily visual cycle.
Dr Ratnayaka added, “This is a further indication of how cells in the eye can deteriorate over time because of these toxic molecules collecting inside RPE cells. This could be a new pathway that no-one has explored before.
Our discoveries have also strengthened the link between diseases of the eye and the brain. The eye is part of the brain and we have shown how Ab which is known to drive major neurological conditions such as Alzheimer’s disease can also causes significant damage to cells in retina.”
The researchers hope that one of the next steps could be for anti-amyloid beta drugs, previously trialled in Alzheimer’s patients, to be re-purposed and trialled as a possible treatment for age-related macular degeneration.
As the regulators in the USA and the European Union have already given approval for many of these drugs, this is an area that could be explored relatively quickly.
The study may also help wider efforts to largely by-pass the use of animal experimentation where possible, so some aspects of testing new clinical treatments can transition directly from cell models to patients.
This research was funded by the National Centre for the Replacement Refinement & Reduction of animals in research (NC3Rs). Dr Katie Bates, Head of Research Funding at the NC3Rs said: ‘This is an impactful study that demonstrates the scientific, practical and 3Rs benefits to studying AMD-like retinal pathology in vitro.’
Animal studies were overseen by the institutions’ Ethical Research Committee and carried out in accordance with the UK Animal (Scientific Procedures) Act of 1986.
Experiments also conformed to the ARVO statement for the Use of Animals in Ophthalmic and Vision Research. The experimental protocol was approved by the University of Southampton Research Ethics Committee and work carried out under the UK Home Office.
more recommended stories
 Pediatric Crohn’s Disease Microbial Signature Identified
Pediatric Crohn’s Disease Microbial Signature IdentifiedKey Points at a Glance NYU.
 High-Fat Diets Cause Damage to Metabolic Health
High-Fat Diets Cause Damage to Metabolic HealthKey Points Takeaways High-fat and ketogenic.
 Can Too Many Antioxidants Harm Future Offspring?
Can Too Many Antioxidants Harm Future Offspring?Key Takeaways High-dose antioxidant supplementation in.
 Human Antibody Drug Response Prediction Gets an Upgrade
Human Antibody Drug Response Prediction Gets an UpgradeKey Takeaways A new humanized antibody.
 Dietary Melatonin Linked to Depression Risk: New Study
Dietary Melatonin Linked to Depression Risk: New StudyKey Summary Cross-sectional analysis of 8,320.
 Type 2 Diabetes Risk Identified by Blood Metabolites
Type 2 Diabetes Risk Identified by Blood MetabolitesKey Takeaways (Quick Summary) Researchers identified.
 Microglia Neuroinflammation in Binge Drinking
Microglia Neuroinflammation in Binge DrinkingKey Takeaways (Quick Summary for HCPs).
 Durvalumab in Small Cell Lung Cancer: Survival vs Cost
Durvalumab in Small Cell Lung Cancer: Survival vs CostKey Points at a Glance Durvalumab.
 Rising Chagas Parasite Detected in Borderland Kissing Bugs
Rising Chagas Parasite Detected in Borderland Kissing BugsKey Takeaways (At a Glance) Infection.
 Can Ketogenic Diets Help PCOS? Meta-Analysis Insights
Can Ketogenic Diets Help PCOS? Meta-Analysis InsightsKey Takeaways (Quick Summary) A Clinical.

Leave a Comment