Though oral health disorders can have an impact on general health, the two are considered unconnected and are typically treated independently. Existing research indicates that people with IBD are more likely to have periodontitis and vice versa, implying a “oral-gut axis” linking the two disorders reciprocally. As a result, collaborative, holistic health care may be a useful treatment option for such people.
A new comprehensive assessment of over 300 papers on the relationship between periodontitis and IBD lends weight to the case. The paper, “Unraveling the Link Between Periodontitis and Inflammatory Bowel Disease: Challenges and Outlook,” is available on the arXiv pre-print service.
Periodontitis is the most severe stage of gum disease, marked by inflamed and receding gums, halitosis, deep periodontal pockets, loose teeth, and tooth loss if ignored. Bacterial plaque buildup on teeth or in the spaces between them causes an inflammatory response in the tooth’s supporting structure, eventually destroying it.
Periodontitis is the most frequent cause of tooth loss in adults worldwide, affecting roughly half of those over the age of 30 and more than 70% of those over the age of 65. Advanced age, diabetes, hereditary factors, certain drugs, poor oral hygiene, and smoking are all risk factors for periodontitis. The disease’s pathogen spread and the systemic inflammation it causes are thought to contribute to other health problems such as diabetes, heart disease, IBD, and premature birth.
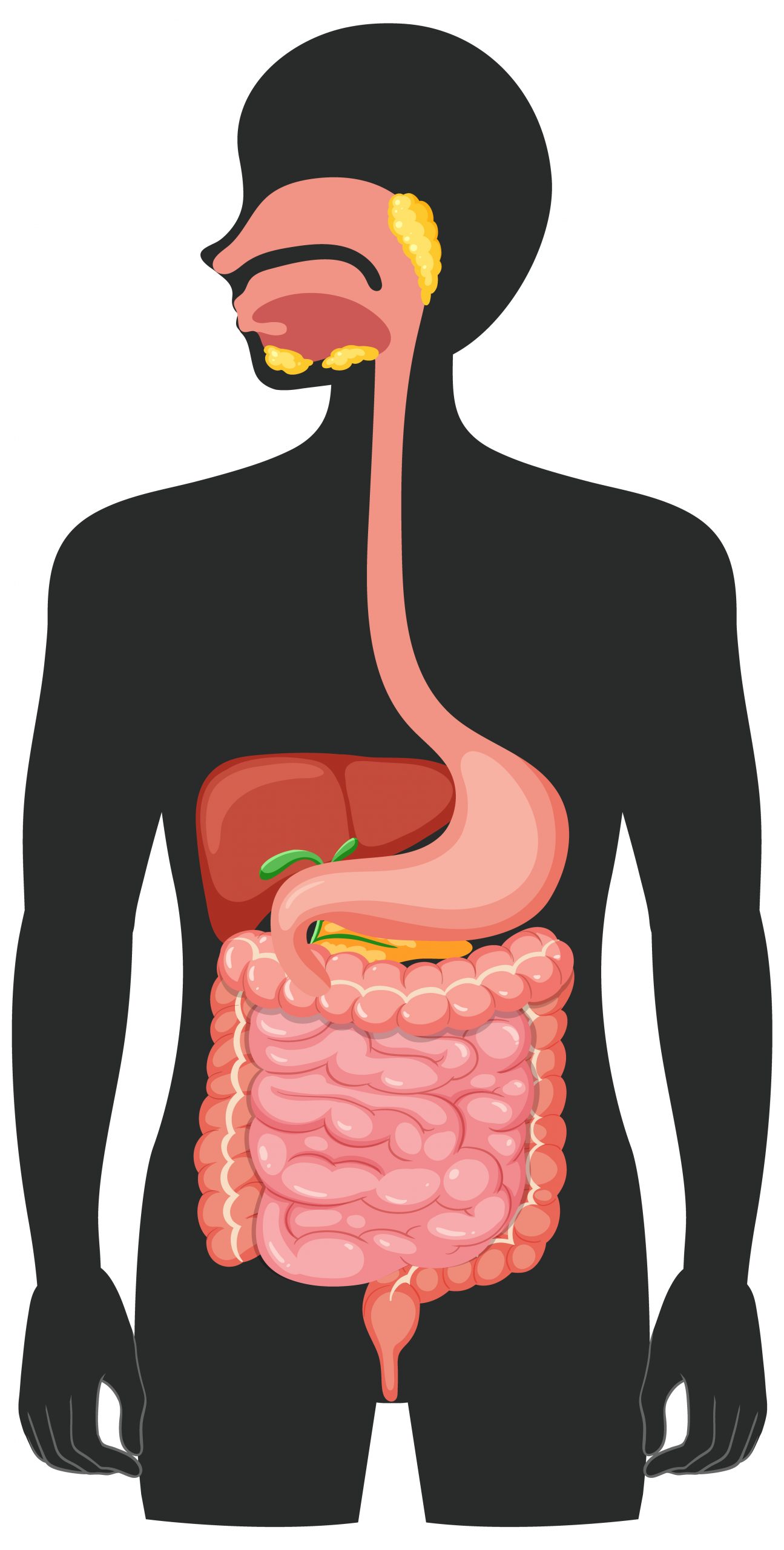
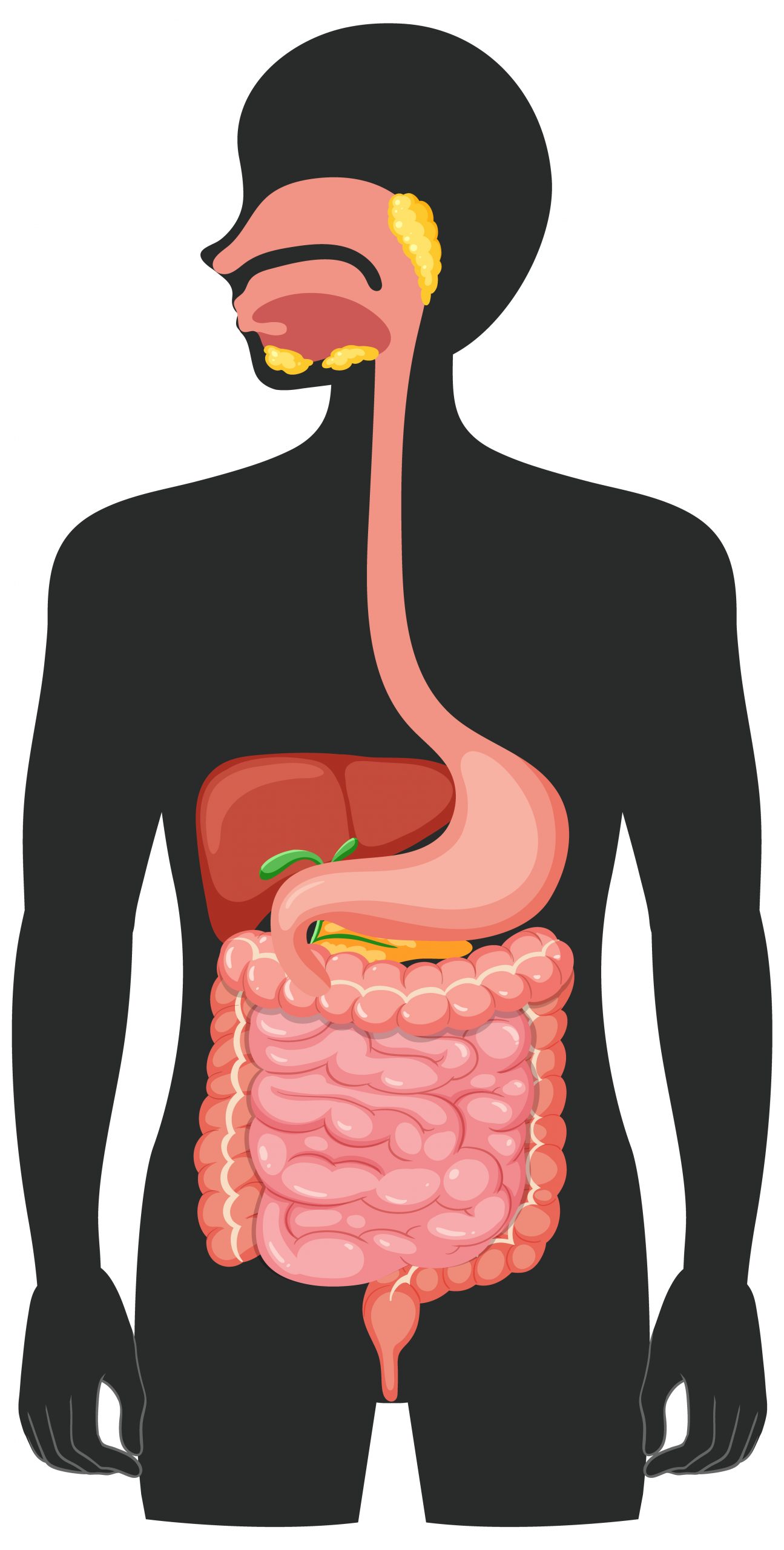
Meanwhile, Crohn’s disease and ulcerative colitis are the two most common types of IBD, a wide group that encompasses a variety of chronic inflammatory disorders affecting the GI tract. Crohn’s disease causes patches of inflammation on the gut wall across both the large and small intestines, whereas ulcerative colitis causes inflammation on the mucosal layer from the colon to the rectum.
Symptoms of both of these inflammatory bowel diseases include stomach pain and cramps, diarrhea, tiredness, fever, nausea and vomiting, and weight loss. Oral lesions are among the main comorbidities seen in 25% to 40% of Crohn’s disease and ulcerative colitis patients.
Although the specific origin of IBD has not been determined, environmental, genetic, and microbial variables, as well as immune responses, are thought to be implicated. Age (it is more prevalent in children and young people, but affects up to 15% of patients beyond the age of 60); ethnicity (it is more common in Caucasians and Ashkenazi Jews); family history; and, specifically for Crohn’s disease, smoking.
Gingivitis (the initial stage of gum disease) and periodontitis, for example, have been reported to impact up to 30% of IBD patients either before, after, or at the same time as GI disorders. Though the exact cause has not been determined, genetics, immune system dysregulation, and changes in the oral microbiome are all thought to have a role.
However, while data suggests a link between IBD and periodontitis, its causation and directionality remain unknown. According to existing studies, a precise sequence of events may be required to induce the development of IBD linked with periodontitis. The new analysis explores the inflammatory responses shared by the two disorders, proposing a “multi-hit model” in which periodontitis and its linked oral bacteria may be involved.
In the future, the study emphasizes the importance of longitudinal research to demonstrate the link between the two situations in greater depth. Notably, it concludes that collaboration among health care professionals and specialists, such as dentists, gastroenterologists, immunologists, and infectious disease experts/microbiologists, is required to provide holistic oral-systemic health care, as well as the reduction of pathogenic oral bacteria to the gut through excellent dental care.
more recommended stories
 Nanoplastics in Brain Tissue and Neurological Risk
Nanoplastics in Brain Tissue and Neurological RiskKey Takeaways for HCPs Nanoplastics are.
 AI Predicts Chronic GVHD Risk After Stem Cell Transplant
AI Predicts Chronic GVHD Risk After Stem Cell TransplantKey Takeaways A new AI-driven tool,.
 Red Meat Consumption Linked to Higher Diabetes Odds
Red Meat Consumption Linked to Higher Diabetes OddsKey Takeaways Higher intake of total,.
 Pediatric Crohn’s Disease Microbial Signature Identified
Pediatric Crohn’s Disease Microbial Signature IdentifiedKey Points at a Glance NYU.
 Nanovaccine Design Boosts Immune Attack on HPV Tumors
Nanovaccine Design Boosts Immune Attack on HPV TumorsKey Highlights Reconfiguring peptide orientation significantly.
 High-Fat Diets Cause Damage to Metabolic Health
High-Fat Diets Cause Damage to Metabolic HealthKey Points Takeaways High-fat and ketogenic.
 Acute Ischemic Stroke: New Evidence for Neuroprotection
Acute Ischemic Stroke: New Evidence for NeuroprotectionKey Highlights A Phase III clinical.
 Statins Rarely Cause Side Effects, Large Trials Show
Statins Rarely Cause Side Effects, Large Trials ShowKey Points at a Glance Large.
 Anxiety Reduction and Emotional Support on Social Media
Anxiety Reduction and Emotional Support on Social MediaKey Summary Anxiety commonly begins in.
 Liquid Biopsy Measures Epigenetic Instability in Cancer
Liquid Biopsy Measures Epigenetic Instability in CancerKey Takeaways Johns Hopkins researchers developed.

Leave a Comment