A recent work lead by the Mead Group and published in Nature Genetics has revealed a hitherto unknown effect of persistent inflammation on TP53-mutant haematopoietic stem cells.
The most frequently altered gene in human malignancies is TP53 (tumor protein 53). The scientists studied the relationship between an aggressive kind of leukemia and TP53 mutations in haematopoietic stem cells in this study.
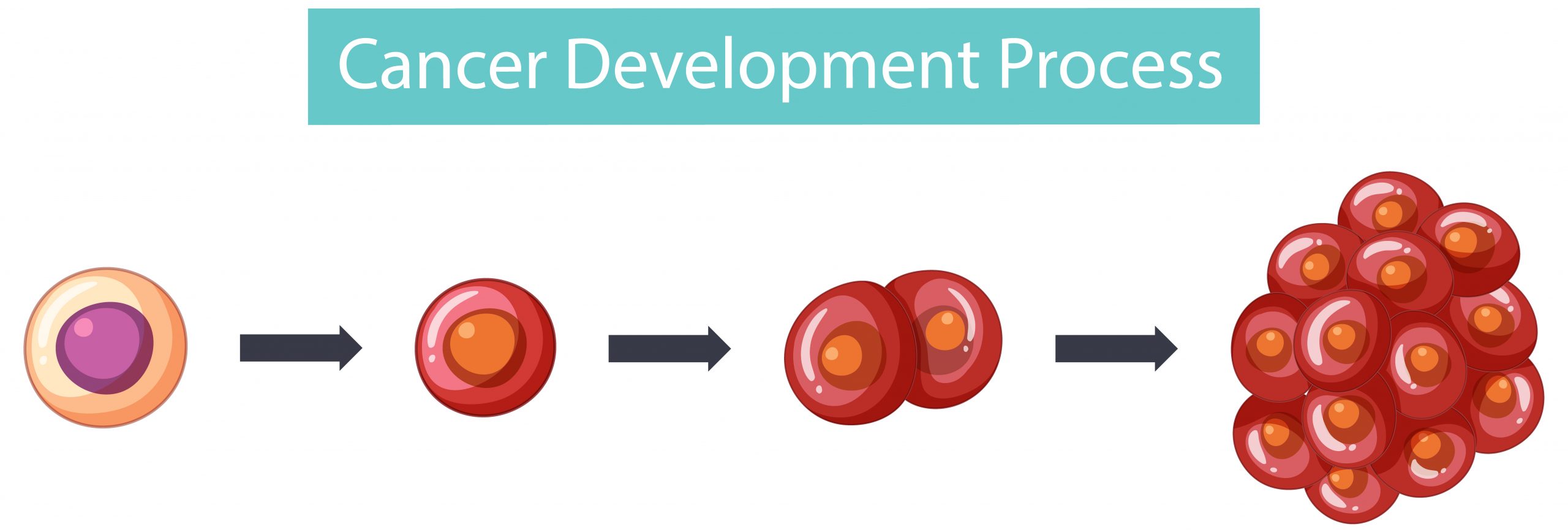
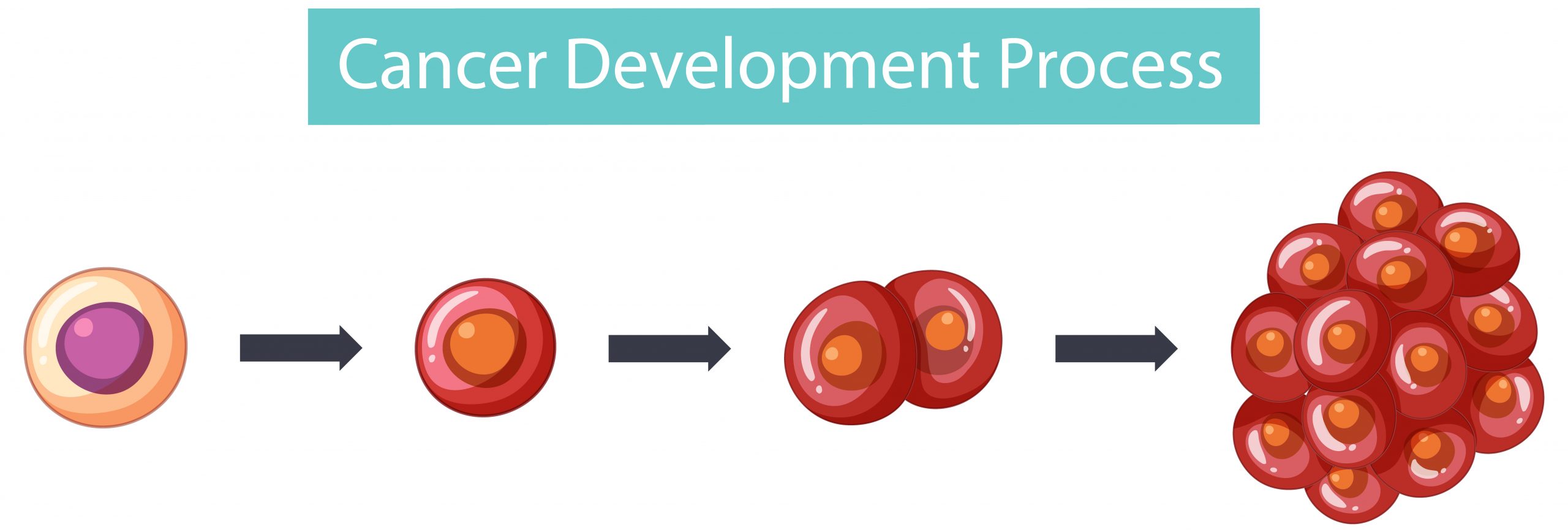
Haematopoietic stem cells (HSCs) may differentiate into all blood cell types, which is necessary for a functional blood system. TP53 mutations in HSCs have previously been linked to a cancer progression pathway that leads to acute myeloid leukemia. The processes by which these TP53-mutated blood stem cells expand and give rise to cancer have remained unknown until now.
INFLAMMATION AND HAEMATOPOIETIC STEM CELLS
When the body detects inflammation, HSCs develop into white blood cells, and the white blood cells produced aid in the fight against the infection. However, in patients with TP53 mutations in their HSCs, inflammation caused selective growth of TP53-mutant cells, which cannot differentiate properly.
TP53 is also known as the “guardian of the genome” because it guarantees that cells do not contain genetic defects; if they do, TP53 initiates a process known as programmed cell death, which inhibits the proliferation of defective stem cells. However, in patients with TP53 deficiency, stem cells are unable to maintain genomic integrity. In this environment, inflammation serves as a tornado, removing normal HSCs from bone marrow while boosting the growth of TP53-mutant cells. This eventually results in a more aggressive form of cancer.
BEING AWARE OF HOW HAEMATOPOIETIC STEM CELLS TURN INTO LEUKEMIC CELLS
The authors of this work, lead by Dr Alba Rodriguez-Meira, Professor Adam Mead (MRC MHU), and Dr Iléana Antony-Debré (Inserm), used a technology created in the Mead group to analyze genetic abnormalities and the genes that are active in each single cell (transcriptome). This technology, known as TARGET-seq, allowed them to identify between HSCs with a TP53 mutation and how they behaved during a patient’s development.
The researchers examined patient-donated cells and observed that TP53-mutant cells from patients who were more likely to acquire leukaemia activated genes involved in inflammatory processes. The authors subsequently demonstrated, using mice, that cells with TP53 mutations increased in frequency when the mice were treated to inflammation.
The authors then investigated the typical effect of inflammation in normal and mutant HSCs. They discovered that TP53-mutant cells produced fewer white blood cells and were resistant to cell death, which is commonly caused by inflammation. This allowed the mutant HSCs to ‘win the race,’ increasing the amount of TP53-mutant cells in the blood.
This study also looked into how well blood stem cells could maintain their genomic integrity in the face of an inflammatory stimuli. The authors discovered that TP53 mutations altered how cells responded to damage in their genetic code, rendering them incapable of properly repairing genetic errors. Some of these genetic abnormalities aided their growth and contributed to cancer formation.
Dr Alba Rodriguez-Meira, one of the paper’s co-first authors, said “Overall, these findings offer valuable insights into how genetic defects and inflammation interact in the development of blood cancer. Importantly, this study could pave the way for better methods of early detection and new treatments for TP53-mutant leukaemia and many other cancer types, improving outcomes for cancer patients.”
Professor Adam Mead, said “I am really proud of this work which illustrates how cutting-edge single-cell techniques can provide novel insights into human disease. The connection between inflammation and genetic evolution in cancer has broad implications and the challenge is now to determine how we might intervene in this process to more effectively treat, or even prevent the inflammation associated with cancer progression. I would like to thank the patients who donated samples to support this research at a very difficult time in their lives and also all coauthors and our funders, particularly CRUK and MRC.”
more recommended stories
 Microglia Neuroinflammation in Binge Drinking
Microglia Neuroinflammation in Binge DrinkingKey Takeaways (Quick Summary for HCPs).
 Precision Oncology with Personalized Cancer Drug Therapy
Precision Oncology with Personalized Cancer Drug TherapyKey Takeaways UC San Diego’s I-PREDICT.
 Iron Deficiency vs Iron Overload in Parkinson’s Disease
Iron Deficiency vs Iron Overload in Parkinson’s DiseaseKey Takeaways (Quick Summary for HCPs).
 Can Ketogenic Diets Help PCOS? Meta-Analysis Insights
Can Ketogenic Diets Help PCOS? Meta-Analysis InsightsKey Takeaways (Quick Summary) A Clinical.
 Silica Nanomatrix Boosts Dendritic Cell Cancer Therapy
Silica Nanomatrix Boosts Dendritic Cell Cancer TherapyKey Points Summary Researchers developed a.
 Vagus Nerve and Cardiac Aging: New Heart Study
Vagus Nerve and Cardiac Aging: New Heart StudyKey Takeaways for Healthcare Professionals Preserving.
 Cognitive Distraction From Conversation While Driving
Cognitive Distraction From Conversation While DrivingKey Takeaways (Quick Summary) Talking, not.
 Fat-Regulating Enzyme Offers New Target for Obesity
Fat-Regulating Enzyme Offers New Target for ObesityKey Highlights (Quick Summary) Researchers identified.
 Spatial Computing Explains How Brain Organizes Cognition
Spatial Computing Explains How Brain Organizes CognitionKey Takeaways (Quick Summary) MIT researchers.
 Gestational Diabetes Risk Identified by Blood Metabolites
Gestational Diabetes Risk Identified by Blood MetabolitesKey Takeaways (Quick Summary for Clinicians).

Leave a Comment