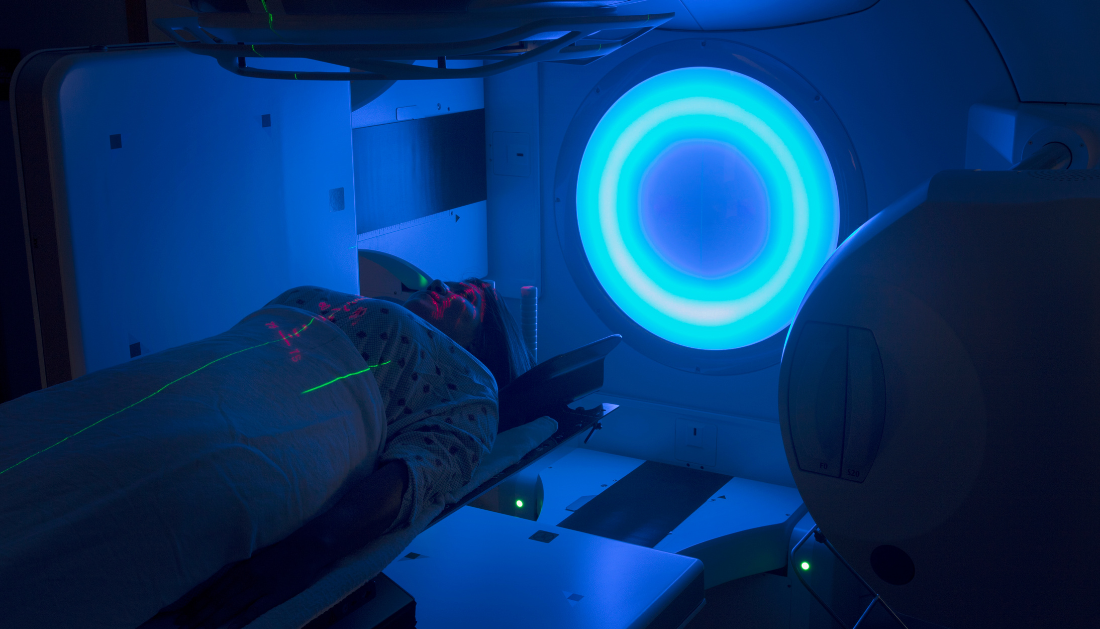
The findings of a phase III trial on a precision radiation approach suggest a “new gold standard” for treating patients with head and neck cancer. According to the research, the novel technique can lower the risk of swallowing issues following radiotherapy while maintaining treatment success.
In the Dysphagia-Aspiration Related Structures (DARS) experiment, dysphagia-optimized intensity-modulated radiation (DO-IMRT) was compared to normal IMRT.
Reducing radiation exposure to swallowing muscles
DO-IMRT optimizes IMRT to lessen the risk of dysphagia, or difficulty swallowing. This common side effect of radiotherapy for head and neck cancer can result in patients requiring a permanent feeding tube in some situations. DO-IMRT reduces the risk of dysphagia by limiting radiation to the pharyngeal muscles that aid in swallowing.
The DARS trial recruited 112 newly diagnosed patients from sites across the United Kingdom and Ireland with oropharyngeal and hypopharyngeal malignancies (tumors of the throat). For six weeks, half of the patients received regular IMRT and the other half received DO-IMRT. The trial’s final results, published in The Lancet Oncology, revealed that:
After two years, patients who had DO-IMRT were more likely to report improved swallowing function than those who received IMRT.
After a year, roughly three-fifths (62%) of DO-IMRT patients reported high normalcy of diet—meaning they could still eat at least some foods that required chewing—and more than eight in ten (85%) said they felt comfortable eating in public, compared to just under 45% and 75% of standard IMRT patients, respectively.
There was no evidence of a difference in survival rates between the two treatments after little over three years of follow-up.
Customized care
Last January, Ian McAllister, 73, of Wandsworth, was diagnosed with oropharyngeal cancer, a type of head and neck cancer. He had dysphagia optimized radiation at The Royal Marsden, which allowed him to avoid the use of a feeding tube. His most recent scan findings revealed no indication of malignancy as well.
“I first noticed something was wrong last summer when I woke up with a numb tongue,” Ian explained. I assumed it was from a hot coffee burn and dismissed it. However, it became scratchy, and by December, I had lost my sense of taste on the left side of my tongue.
“I was diagnosed with cancer shortly after Christmas after undergoing tests at my local hospital.” The tumor was staged as T4 and had expanded to my lymph nodes on both sides, soft palate, and was wrapped around my left tonsil.
“I was referred to The Royal Marsden Hospital and informed that I would require radiotherapy.” My team had informed me that the procedure could result in me having a feeding tube, which would have limited me to liquid or pureed food. However, I understand that my treatment was designed to help reduce the risk of this happening, which is excellent.
“I thought radiotherapy was a breeze for the first couple of weeks, but the side effects mounted.” By week four, I had lost my sense of taste and my saliva glands had ceased functioning, making eating a great challenge. However, because to this optimized radiotherapy and the dieticians and speech and language therapists at The Royal Marsden who helped me with meal planning, mouth exercises, and buckets of encouragement, I was able to play golf three weeks after finishing treatment. I no longer have difficulty swallowing, and while my taste and saliva glands have not yet returned, I am certain that my rehabilitation will allow me to do so.”
‘A new gold standard,’ they say.
“The final results from this study support a new gold standard for treating head and neck cancer patients with radiotherapy,” said study lead Professor Chris Nutting, consultant clinical oncologist at The Royal Marsden NHS Foundation Trust and Professor of Radiation Oncology at The Institute of Cancer Research, London. We have shown that this tailored form of radiation can spare patients’ swallowing muscles while maintaining treatment success.
“In this approach, oncologists and physicists spend more time designing the treatment based on the size and location of the tumor.” A computer will then arrange the dose and route, dividing the radiation into several smaller, more precise beams that will assist protect the throat where possible. We anticipate that additional facilities will adopt this technique because these therapy modifications can considerably improve quality of life.”
“The vast majority of patients I support have had a head and neck cancer diagnosis, and many unfortunately experience swallowing problems during and after treatment, which often includes radiotherapy,” said Professor Justin Roe, consultant speech and language therapist and joint head of the Department of Speech, Voice, and Swallowing at The Royal Marsden NHS Foundation Trust. I frequently see people who no longer enjoy food and drink or who are too embarrassed to consume them in public, which can lead to sadness and isolation.
“Dysphagia can also lead to serious medical complications such as malnutrition, dehydration, and, in some cases, respiratory complications.” It has been an honor to support this research, and I hope that many more patients will benefit from this personalized form of radiotherapy in the future.”
‘Advanced radiotherapy’
“Maintaining the ability to eat and drink normally following treatment for head and neck cancer is incredibly important for patients’ well-being,” said Professor Emma Hall, Co-Director of the Clinical Trials and Statistics Unit at The Institute of Cancer Research, London, which coordinated the trial. We’re thrilled that our experiment shown that we can modify how we deliver cutting-edge radiotherapy to limit damage to essential swallowing muscles and structures, allowing more people to continue to enjoy eating and drinking after treatment.
“This is just one example of how advanced radiotherapy techniques like Do-IMRT can help more patients live well, with fewer side effects, after receiving cancer treatment.”
“Behind the results of each clinical trial, there are real people who deserve the best possible quality of life,” said Martin Ledwick, Cancer Research UK’s lead nurse. It is critical that the treatments not only function, but are also gentle enough to allow them to enjoy life’s pleasures.
“It’s difficult for many of us to imagine not being able to swallow properly, but this is a possibility for patients with head and neck cancer after treatment.”
“These promising results could make life after treatment brighter for head and neck cancer patients, and we look forward to seeing this kinder form of radiotherapy make its way to the clinic.”
more recommended stories
 Microglia Neuroinflammation in Binge Drinking
Microglia Neuroinflammation in Binge DrinkingKey Takeaways (Quick Summary for HCPs).
 Precision Oncology with Personalized Cancer Drug Therapy
Precision Oncology with Personalized Cancer Drug TherapyKey Takeaways UC San Diego’s I-PREDICT.
 Iron Deficiency vs Iron Overload in Parkinson’s Disease
Iron Deficiency vs Iron Overload in Parkinson’s DiseaseKey Takeaways (Quick Summary for HCPs).
 Can Ketogenic Diets Help PCOS? Meta-Analysis Insights
Can Ketogenic Diets Help PCOS? Meta-Analysis InsightsKey Takeaways (Quick Summary) A Clinical.
 Silica Nanomatrix Boosts Dendritic Cell Cancer Therapy
Silica Nanomatrix Boosts Dendritic Cell Cancer TherapyKey Points Summary Researchers developed a.
 Vagus Nerve and Cardiac Aging: New Heart Study
Vagus Nerve and Cardiac Aging: New Heart StudyKey Takeaways for Healthcare Professionals Preserving.
 Cognitive Distraction From Conversation While Driving
Cognitive Distraction From Conversation While DrivingKey Takeaways (Quick Summary) Talking, not.
 Fat-Regulating Enzyme Offers New Target for Obesity
Fat-Regulating Enzyme Offers New Target for ObesityKey Highlights (Quick Summary) Researchers identified.
 Spatial Computing Explains How Brain Organizes Cognition
Spatial Computing Explains How Brain Organizes CognitionKey Takeaways (Quick Summary) MIT researchers.
 Gestational Diabetes Risk Identified by Blood Metabolites
Gestational Diabetes Risk Identified by Blood MetabolitesKey Takeaways (Quick Summary for Clinicians).

Leave a Comment