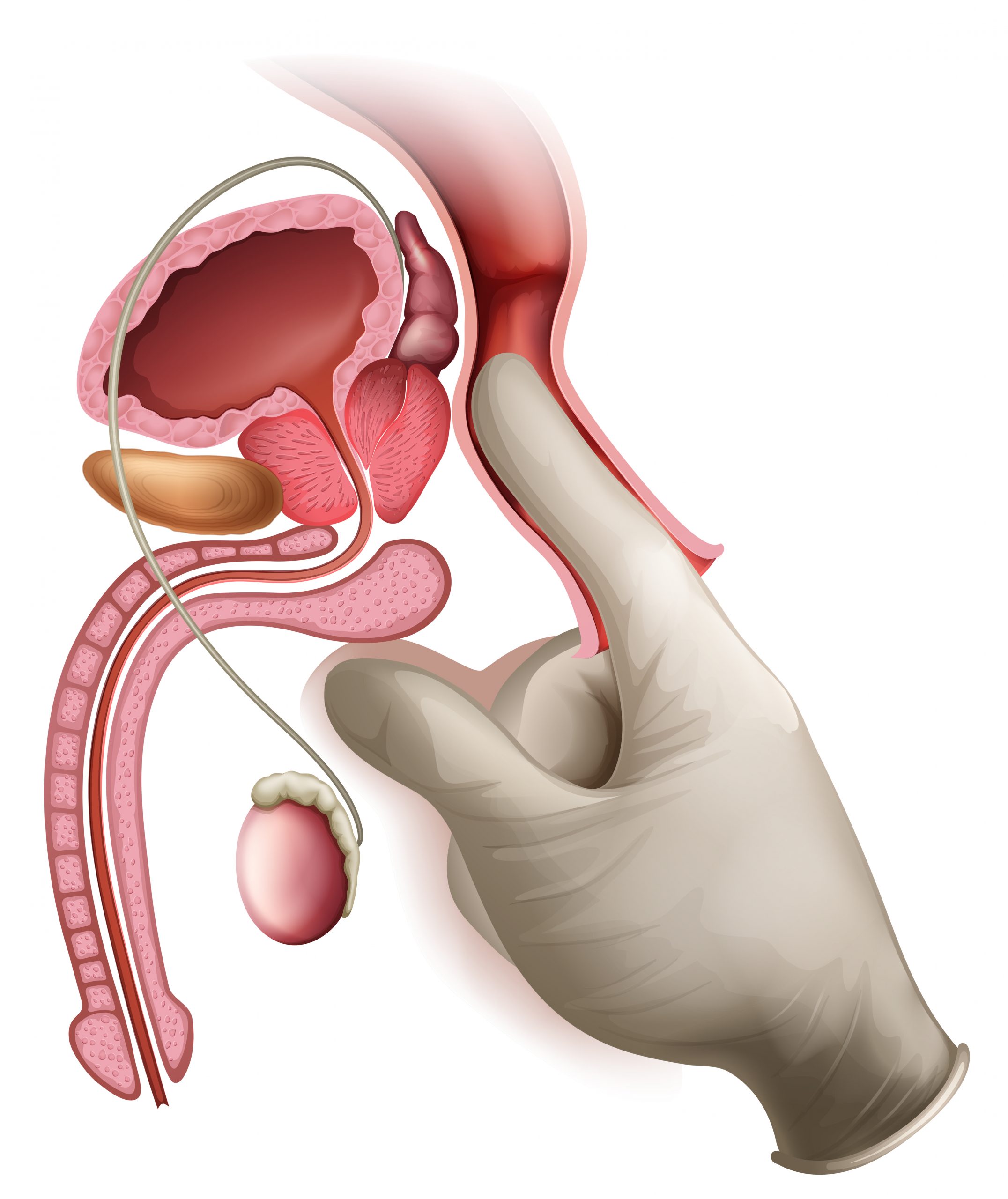
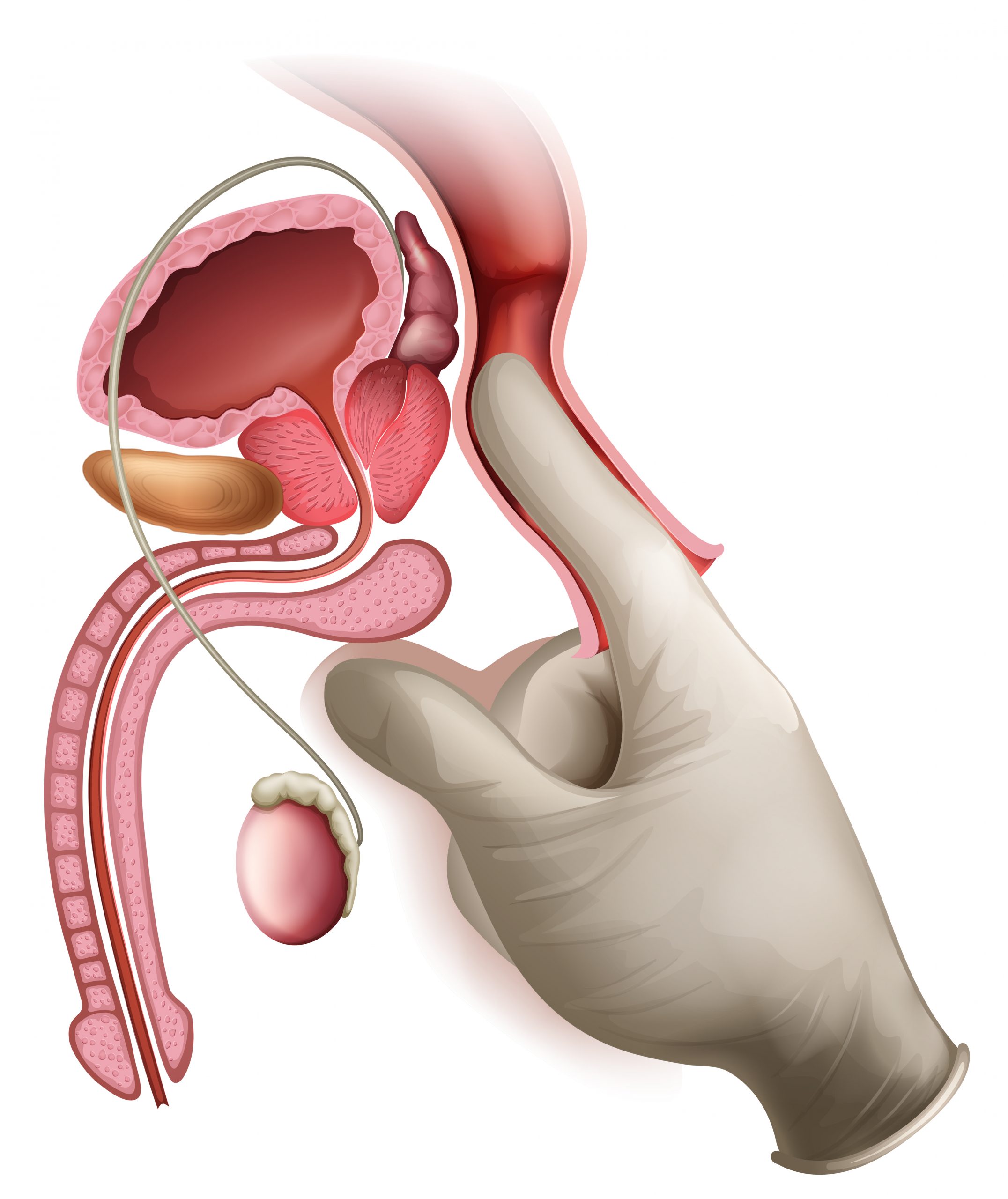
Prostate cancer is the most common type of cancer in males and the second greatest cause of cancer death in the United States. The persistent disease can continue to grow in its ever-indelicate environment even when the amount of testosterone in the body is decreased to very low levels, earning the clunky moniker castrate-resistant prostate cancer (CRPC). It poses a significant clinical issue since a protein known as the androgen receptor (AR) remains a key participant in cancer, modifying its behavior in CRPCs.
Androgen-deprivation therapy, which lowers male hormone levels, is the first-line treatment for locally progressed or metastatic prostate cancer. Regardless of initial responses to medication, nearly all patients develop CRPC within a few years. It is now widely acknowledged that CRPC remains dependent on AR signaling.
“Understanding the triggers that cause changes in AR’s activity is important for developing better treatments for CRPCs,” said Ping Yi, assistant professor of biology and biochemistry, who is leading a team investigating CRPC. Yi’s research is published in PNAS.
Ramesh Singh, Lance Lumahan, and Hong Shen from Baylor College of Medicine’s Department of Molecular and Cellular Biology; and Steven Nguyen from the University of Houston’s Department of Biology and Biochemistry, Center for Nuclear Receptors and Cell Signaling.
“We found a specific chemical modification that occurs on the AR protein in certain conditions where the levels of male hormones are reduced to castration conditions. This modification involves another protein called TRAF4, which is frequently overexpressed in advanced prostate cancers. We demonstrated that overexpression of TRAF4 leads to the conversion of androgen-sensitive prostate cancer cells into castration-resistant cells, both in lab experiments and in live samples,” said Yi.
“We also found that the TRAF4 protein level is higher in androgen-insensitive lymph node carcinoma cells of the prostate.”
TRAF4 is also linked to the spread of cancer to other regions of the body, according to the research. Yi studied cells from patients with metastatic cancer who had previously had androgen-deprivation therapy for this study. The TRAF4 protein was also shown to be higher in cancer cells that are no longer susceptible to androgens compared to cells that are still receptive to androgens.
The researchers feel that these findings give a solid foundation for identifying a subset of CRPC patients who may benefit from a medication that targets the specific molecular changes produced by the AR mutation, potentially giving a treatment option for this group of patients.
more recommended stories
 Red Meat Consumption Linked to Higher Diabetes Odds
Red Meat Consumption Linked to Higher Diabetes OddsKey Takeaways Higher intake of total,.
 Pediatric Crohn’s Disease Microbial Signature Identified
Pediatric Crohn’s Disease Microbial Signature IdentifiedKey Points at a Glance NYU.
 Nanovaccine Design Boosts Immune Attack on HPV Tumors
Nanovaccine Design Boosts Immune Attack on HPV TumorsKey Highlights Reconfiguring peptide orientation significantly.
 High-Fat Diets Cause Damage to Metabolic Health
High-Fat Diets Cause Damage to Metabolic HealthKey Points Takeaways High-fat and ketogenic.
 Acute Ischemic Stroke: New Evidence for Neuroprotection
Acute Ischemic Stroke: New Evidence for NeuroprotectionKey Highlights A Phase III clinical.
 Statins Rarely Cause Side Effects, Large Trials Show
Statins Rarely Cause Side Effects, Large Trials ShowKey Points at a Glance Large.
 Anxiety Reduction and Emotional Support on Social Media
Anxiety Reduction and Emotional Support on Social MediaKey Summary Anxiety commonly begins in.
 Liquid Biopsy Measures Epigenetic Instability in Cancer
Liquid Biopsy Measures Epigenetic Instability in CancerKey Takeaways Johns Hopkins researchers developed.
 Human Antibody Drug Response Prediction Gets an Upgrade
Human Antibody Drug Response Prediction Gets an UpgradeKey Takeaways A new humanized antibody.
 Pancreatic Cancer Research: Triple-Drug Therapy Success
Pancreatic Cancer Research: Triple-Drug Therapy SuccessKey Summary Spanish researchers report complete.

Leave a Comment