According to a study led by Weill Cornell Medicine, NewYork-Presbyterian, and Yale School of Medicine researchers, a common type of brain bleed in older persons known as subdural hemorrhage is connected with the presence of amyloid deposits in cerebral blood vessels. The research is the first to link cerebral vascular amyloid to subdural hemorrhages, and it should help researchers better understand both disorders.
The researchers evaluated two large population-based cohorts comprising more than 600,000 adults in the United Kingdom and the United States for the study, which appears in JAMA Neurology on December 26. They discovered that individuals who had amyloid deposits in their cerebral vessels, a disorder known as cerebral amyloid angiopathy (CAA), were at least five times more likely to have subdural hemorrhages than those who did not have CAA.
“At present, clinicians generally don’t consider isolated subdural hemorrhages as part of the spectrum of cerebral amyloid angiopathy. So, if this link is established, then clinicians will start to screen and evaluate subdural hemorrhage patients for underlying CAA, which would be a major paradigm shift and could lead to better care and better outcomes.”- Dr. Santosh Murthy, study co-senior author, associate professor of neurology at Weill Cornell Medicine and the associate chief of the division of neurocritical care at New York-Presbyterian/Weill Cornell Medical Center
Dr. Guido Falcone, an associate professor of neurology at Yale School of Medicine, was also a co-senior author on the study. Dr. Cyprien Rivier, a postdoctoral associate in the Falcone laboratory, was the study’s primary author.
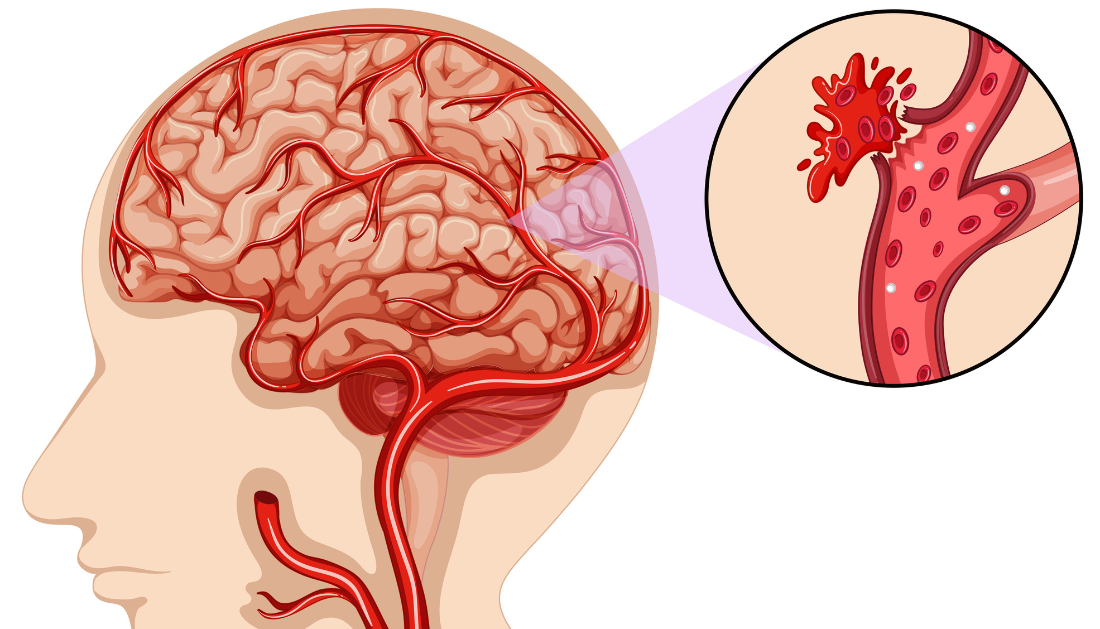
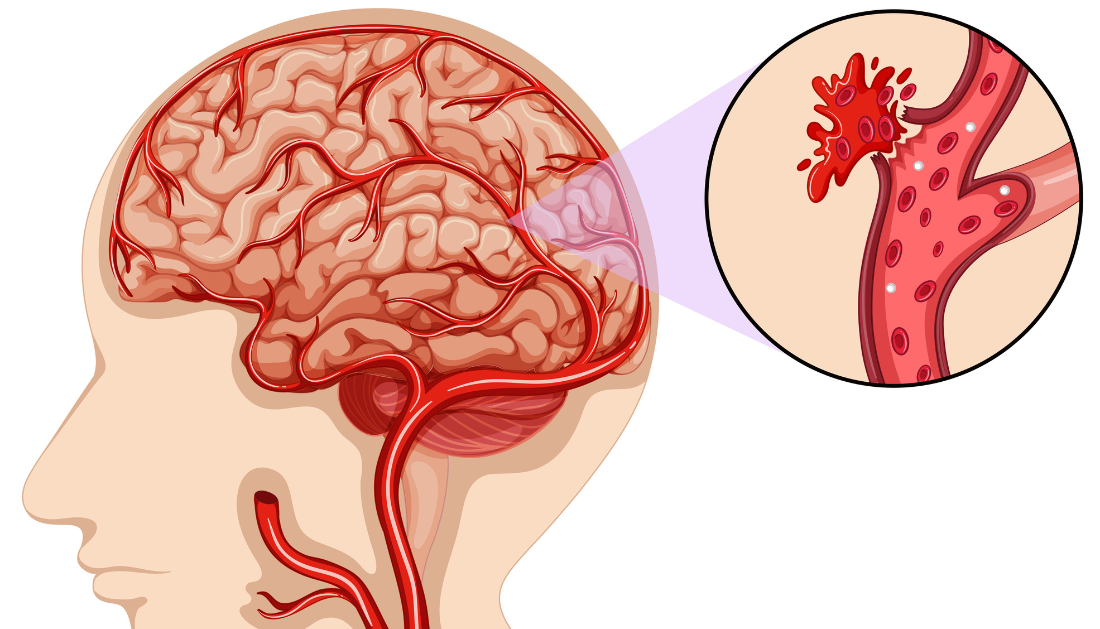
Subdural hemorrhages are bleeds from blood vessels on the brain’s outer surface, beneath its greatest covering membrane, the dura. They cause trapped blood, known as subdural hematomas, which can place hazardous pressure on the brain and usually necessitate surgical removal. Subdural hemorrhages harm roughly 125,000 Americans each year and, as the population ages, are on their way to becoming the most prevalent reason for adult brain surgery.
CAA is characterized by amyloid beta protein clumps in blood vessel walls within and slightly above the brain. The disorder is highly common in older people, particularly Alzheimer’s patients who have amyloid deposits in other brain areas. Although CAA can cause bleeding from any of the veins in which it is present, neurologists have long considered subdural hemorrhage to be a unique clinical phenomena caused mostly by mechanical strains on vessels caused by age-related brain shrinkage.
Nonetheless, there have been signs of a link between the two. One-fifth of CAA brain bleed patients also have subdural hemorrhages, and there is some indication that subdural hemorrhages are more likely when CAA symptoms are more visible on brain MRI images. As a result, Drs. Murthy and Falcone, along with their colleagues, established the new study as a first investigation of this potential link.
They used data from the New York City Consortium of Columbia University Irving Medical Center, Weill Cornell Medicine, NYC Health + Hospitals/Harlem, and NewYork-Presbyterian to conduct their analysis, as well as data from two ongoing, long-term, population-based health studies, the UK’s Biobank Program and the US National Institutes of Health’s All of Us Research Program. They evaluated the rates of subdural hemorrhages in patients with and without a prior CAA diagnosis in datasets spanning a total of 645,231 participants.
During a median follow-up period of about 20 years, 3 of the 126 persons with CAA and 649 of the 487,097 people without CAA suffered a subdural hemorrhage in the broader UK-based dataset. According to the researchers’ calculations, this meant that the CAA group had a 7.6 times higher chance of subdural hemorrhage. Confirming the association, the researchers calculated a 5.2-fold increase in risk for CAA patients in the US sample.
While the authors noted that this apparent statistical correlation does not prove that CAA causes subdural hemorrhages, it does motivate more research.
“The next logical step is to do a multicenter prospective study looking for the presence of amyloid using PET scans in patients who present with an isolated subdural hemorrhage,” said Dr. Murthy.
There are currently no particular therapies for CAA. Anti-amyloid treatments, which were recently approved for use in Alzheimer’s disease, may be investigated in CAA patients in the future. In theory, however, screening subdural hemorrhage patients for CAA could identify many patients who would benefit from such treatments when they become accessible, according to Dr. Murthy.
For more information: Cerebral Amyloid Angiopathy and Risk of Isolated Nontraumatic Subdural Hemorrhage, JAMA Network, https://doi.org/10.1001/jamaneurol.2023.4918
more recommended stories
 CTNNB1 Syndrome Study Explores Beta-Catenin Defects
CTNNB1 Syndrome Study Explores Beta-Catenin DefectsKey Takeaways Researchers in Spain are.
 Tuberculosis Breakthrough with Experimental Antibiotics
Tuberculosis Breakthrough with Experimental AntibioticsKey Takeaways Experimental antibiotics disrupt a.
 National Healthy Longevity Trial Receives Federal Support
National Healthy Longevity Trial Receives Federal SupportKey Summary Up to $38 million.
 Red Blood Cells Improve Glucose Tolerance Under Hypoxia
Red Blood Cells Improve Glucose Tolerance Under HypoxiaKey Takeaways for Clinicians Chronic hypoxia.
 Nanoplastics in Brain Tissue and Neurological Risk
Nanoplastics in Brain Tissue and Neurological RiskKey Takeaways for HCPs Nanoplastics are.
 AI Predicts Chronic GVHD Risk After Stem Cell Transplant
AI Predicts Chronic GVHD Risk After Stem Cell TransplantKey Takeaways A new AI-driven tool,.
 Red Meat Consumption Linked to Higher Diabetes Odds
Red Meat Consumption Linked to Higher Diabetes OddsKey Takeaways Higher intake of total,.
 Pediatric Crohn’s Disease Microbial Signature Identified
Pediatric Crohn’s Disease Microbial Signature IdentifiedKey Points at a Glance NYU.
 Nanovaccine Design Boosts Immune Attack on HPV Tumors
Nanovaccine Design Boosts Immune Attack on HPV TumorsKey Highlights Reconfiguring peptide orientation significantly.
 High-Fat Diets Cause Damage to Metabolic Health
High-Fat Diets Cause Damage to Metabolic HealthKey Points Takeaways High-fat and ketogenic.

Leave a Comment