

The FDA approved Lenmeldy (atidarsagene autotemcel) today, making it the first FDA-approved gene therapy for the treatment of children with pre-symptomatic late infantile, pre-symptomatic early juvenile, or early symptomatic early juvenile metachromatic leukodystrophy.
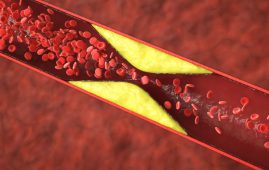
Metachromatic leukodystrophy is a devastating, uncommon hereditary condition that affects the brain and nervous system. A lack of an enzyme known as arylsulfatase A (ARSA) causes an accumulation of sulfatides (fatty compounds) in cells. This buildup causes harm to the central and peripheral nerve systems, resulting in loss of motor and cognitive function and premature death. It is believed that Metachromatic Leukodystrophy affects one out of every 40,000 people in the United States. There is no cure for MLD, and therapy is typically limited to supportive care and symptom control.
“This is the first FDA-approved treatment option for children who have this rare genetic disease,” says Peter Marks, M.D., Ph.D., director of the FDA’s Center for Biologics Evaluation and Research. “We remain committed to advancing scientific and regulatory principles that enable the efficient development and review of safe, effective and innovative products that have the potential to change patients’ lives.”
Lenmeldy is a one-time, customized, single-dose infusion generated from the patient’s own hematopoietic (blood) stem cells (HSCs) that have been genetically engineered to contain functioning ARSA genes. The patient’s stem cells are harvested and transformed to include a functional copy of the ARSA gene. The transformed stem cells are reintroduced into the patient, where they engraft (attach and multiply) in the bone marrow. The modified stem cells provide the body with myeloid (immune) cells that generate the ARSA enzyme, which aids in the breakdown of toxic sulfatide buildup and may slow the progression of MLD. Prior to treatment, patients must endure high-dose chemotherapy, a technique that eliminates cells from the bone marrow and replaces them with the modified cells in Lenmeldy.
“MLD is a devastating disease that profoundly affects the quality of life of patients and their families. Advancements in treatment options offer hope for improved outcomes and the potential to positively influence the trajectory of disease progression,” says Nicole Verdun, M.D., director of the Office of Therapeutic Products at CBER. “This approval represents important progress in the advancement and availability of effective treatments, including gene therapies, for rare diseases.”
The safety and efficacy of Lenmeldy were evaluated using data from 37 children who received it in two single-arm, open-label clinical studies and an expanded access program. Child treated with Lenmeldy were compared to untreated children (natural history). The primary effectiveness objective was severe motor impairment-free survival, which was defined as the time between birth and the first loss of locomotion, loss of sitting without assistance, or death. In children with MLD, Lenmeldy medication dramatically reduced the probability of severe motor impairment or mortality when compared to untreated children. All infants with pre-symptomatic late infantile MLD who were treated with Lenmeldy survived to the age of six, whereas only 58% of children in the natural history group did.
At five years old, 71% of treated youngsters could walk without assistance. Eighty-five percent of the children treated had normal language and performance IQ levels, which had not previously been documented in untreated children.
Furthermore, children with pre-symptomatic and early symptomatic early juvenile MLD had a slower progression of motor and/or cognitive pathology.
Lenmeldy’s most common side effects are fever, low white blood cell count, mouth sores, respiratory infections, rash, medical line infections, viral infections, fever, gastrointestinal infections, and an enlarged liver.
After receiving Lenmeldy, patients should be monitored for neutrophil counts and the likelihood of delayed platelet engraftment until engraftment occurs.Lenmeldy treatment may result in the production of blood clots or encephalitis, a type of brain tissue swelling. There is a risk of blood cancer connected with this medication, however, no incidences have been reported in people treated with Lenmeldy. Patients who receive this medication should be monitored for hematologic malignancies for the rest of their lives, including a complete blood count (with differential) once a year and integration site examination as needed for at least 15 years after therapy.
more recommended stories
 Children’s Health in the United States is Declining!
Children’s Health in the United States is Declining!Summary: A comprehensive analysis of U.S..
 Autoimmune Disorders: ADA2 as a Therapeutic Target
Autoimmune Disorders: ADA2 as a Therapeutic TargetAdenosine deaminase 2 (ADA2) has emerged.
 Is Prediabetes Reversible through Exercise?
Is Prediabetes Reversible through Exercise?150 Minutes of Weekly Exercise May.
 New Blood Cancer Model Unveils Drug Resistance
New Blood Cancer Model Unveils Drug ResistanceNew Lab Model Reveals Gene Mutation.
 Healthy Habits Slash Diverticulitis Risk in Half: Clinical Insights
Healthy Habits Slash Diverticulitis Risk in Half: Clinical InsightsHealthy Habits Slash Diverticulitis Risk in.
 Caffeine and SIDS: A New Prevention Theory
Caffeine and SIDS: A New Prevention TheoryFor the first time in decades,.
 Microbial Metabolites Reveal Health Insights
Microbial Metabolites Reveal Health InsightsThe human body is not just.
 Reelin and Cocaine Addiction: A Breakthrough Study
Reelin and Cocaine Addiction: A Breakthrough StudyA groundbreaking study from the University.
 Preeclampsia and Stroke Risk: Long-Term Effects
Preeclampsia and Stroke Risk: Long-Term EffectsPreeclampsia (PE) – a hypertensive disorder.
 Statins and Depression: No Added Benefit
Statins and Depression: No Added BenefitWhat Are Statins Used For? Statins.

Leave a Comment