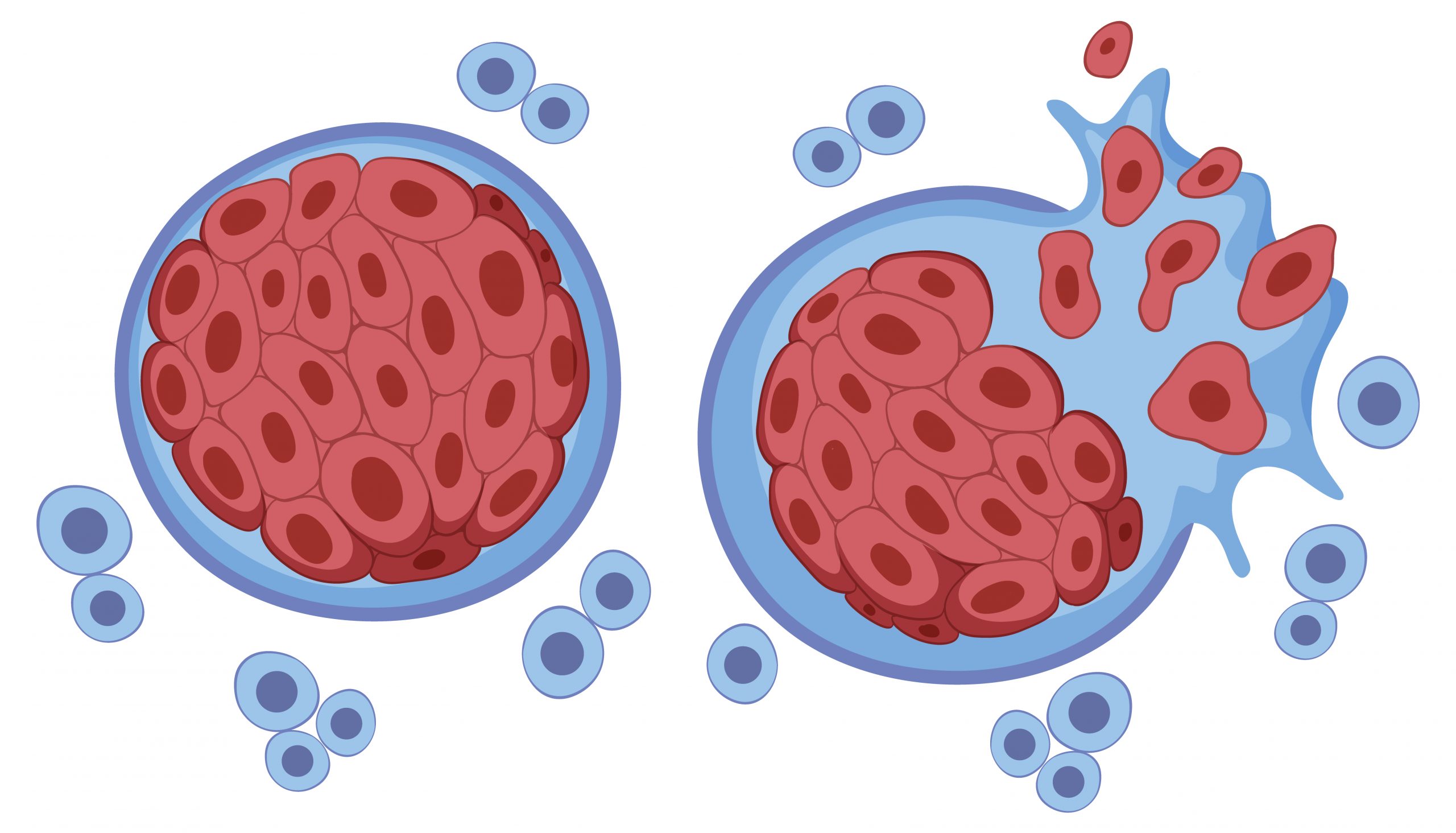
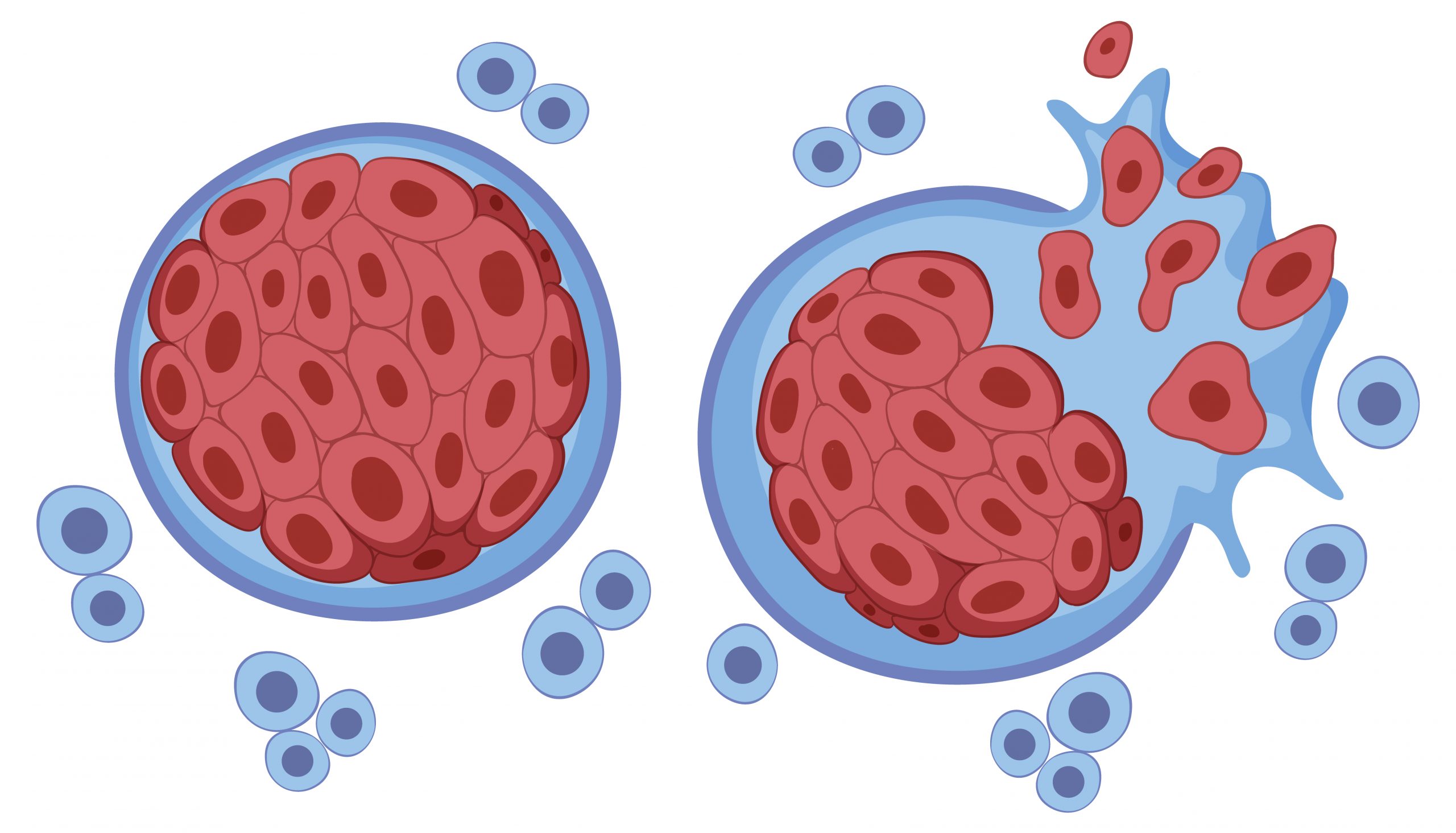
T cells in the immune system that should be able to kill cancer cells become ineffective or “exhausted” within hours of coming into contact with a tumor, according to a study published Aug. 3 in Nature Immunology.
According to Mary Philip, MD, Ph.D., assistant professor of Medicine in the Division of Hematology and Oncology at Vanderbilt University Medical Center, the surprising findings have implications for cancer immunotherapies that aim to harness the tumor-killing power of T cells, and they challenge existing ideas about how T cells become exhausted.
“The idea has been that T cells that are exposed to an antigen (such as a tumor or pathogen) for a long time are working and working, and then at some point they sort of peter out. That’s where the term exhaustion comes from,” said Philip, senior author of the study.
“I don’t think anyone expected that within six to 12 hours, T cells would look dysfunctional or exhausted; that’s a very fast time window.”
Philip and her colleagues utilized their previously established genetic mouse model, in which mice acquire liver tumors as they age in a manner similar to human patients, to investigate how T cells become tired and discover targets that could prevent or reverse it. The researchers may analyze how trackable T cells respond to established malignancies and track immune responses as cancers develop.
“In patients who are diagnosed with cancer, we can’t go back in time to find out how the immune system responded,” Philip said. “The mouse model allows us to do this, to say, “What is happening when T cells first see tumors; when and how do the T cells get exhausted?”
Researchers can evaluate how T cells respond to malignancies versus infection in parallel experiments. T cells become functional in the context of acute infection, but dysfunctional in the context of malignancies, explains Philip.
“This comparison allows us to compare what a ‘good’ T cell looks like versus a dysfunctional T cell,” she said.
In a prior series of studies published in 2016 and 2017, researchers discovered that tumor-activated T cells were dysfunctional after only five days and had thousands of changes in genes that are switched on or off when compared to infection-activated T cells.
The current research, directed by Michael Rudloff, Ph.D., a Medical Scientist Training Program student, looked back in time. They hoped to uncover fewer differences between infection-activated and tumor-activated T cells, which could point to crucial genes or signaling pathways that could be targeted to make dysfunctional T cells ‘good’ again. Instead, within six to twelve hours, they discovered all of the hallmarks of T cell exhaustion, including substantial alterations in chromatin accessibility and gene expression.
“We still have thousands of different genes to look at,” Philip said.
Despite the absence of a few important targets, the researchers discovered several tendencies, such as increased expression of inflammation-associated genes and transcription factors during infection, which are not activated in the tumor model. They are now investigating infection and other methods of stimulating innate immune pathways in order to improve T cell performance.
Other significant findings of the current investigation include:
- T cells were stimulated and divided following tumor exposure, although functional alterations were observed prior to cell division, which was anticipated.
- T cells in a metastatic melanoma model became dysfunctional within hours as well, suggesting that the modifications are not tumor-specific.
- T cells isolated from the tumor after five days or more and transplanted to a tumor-free mice did not regain function, implying that the modifications are “imprinted.”
- T cells that had been fully activated and functional before being placed into the tumor model turned dysfunctional, demonstrating that negative tumor signals can override functional programs.
The researchers were able to uncover indicators from these and other studies that allow them to predict whether T cells will respond to a tumor or not, which could assist personalize immunotherapies.
We know that checkpoint inhibitors and other immunotherapy interventions don’t work in a lot of patients, and it’s important to be able to predict response and avoid therapies that won’t benefit patients,” Philip said.
more recommended stories
 Nanoplastics in Brain Tissue and Neurological Risk
Nanoplastics in Brain Tissue and Neurological RiskKey Takeaways for HCPs Nanoplastics are.
 AI Predicts Chronic GVHD Risk After Stem Cell Transplant
AI Predicts Chronic GVHD Risk After Stem Cell TransplantKey Takeaways A new AI-driven tool,.
 Red Meat Consumption Linked to Higher Diabetes Odds
Red Meat Consumption Linked to Higher Diabetes OddsKey Takeaways Higher intake of total,.
 Pediatric Crohn’s Disease Microbial Signature Identified
Pediatric Crohn’s Disease Microbial Signature IdentifiedKey Points at a Glance NYU.
 Nanovaccine Design Boosts Immune Attack on HPV Tumors
Nanovaccine Design Boosts Immune Attack on HPV TumorsKey Highlights Reconfiguring peptide orientation significantly.
 High-Fat Diets Cause Damage to Metabolic Health
High-Fat Diets Cause Damage to Metabolic HealthKey Points Takeaways High-fat and ketogenic.
 Acute Ischemic Stroke: New Evidence for Neuroprotection
Acute Ischemic Stroke: New Evidence for NeuroprotectionKey Highlights A Phase III clinical.
 Statins Rarely Cause Side Effects, Large Trials Show
Statins Rarely Cause Side Effects, Large Trials ShowKey Points at a Glance Large.
 Anxiety Reduction and Emotional Support on Social Media
Anxiety Reduction and Emotional Support on Social MediaKey Summary Anxiety commonly begins in.
 Liquid Biopsy Measures Epigenetic Instability in Cancer
Liquid Biopsy Measures Epigenetic Instability in CancerKey Takeaways Johns Hopkins researchers developed.

Leave a Comment