Scientists have uncovered an odd discovery that could aid in the identification of people who are up to two and a half times more likely to respond to currently available cancer treatment.
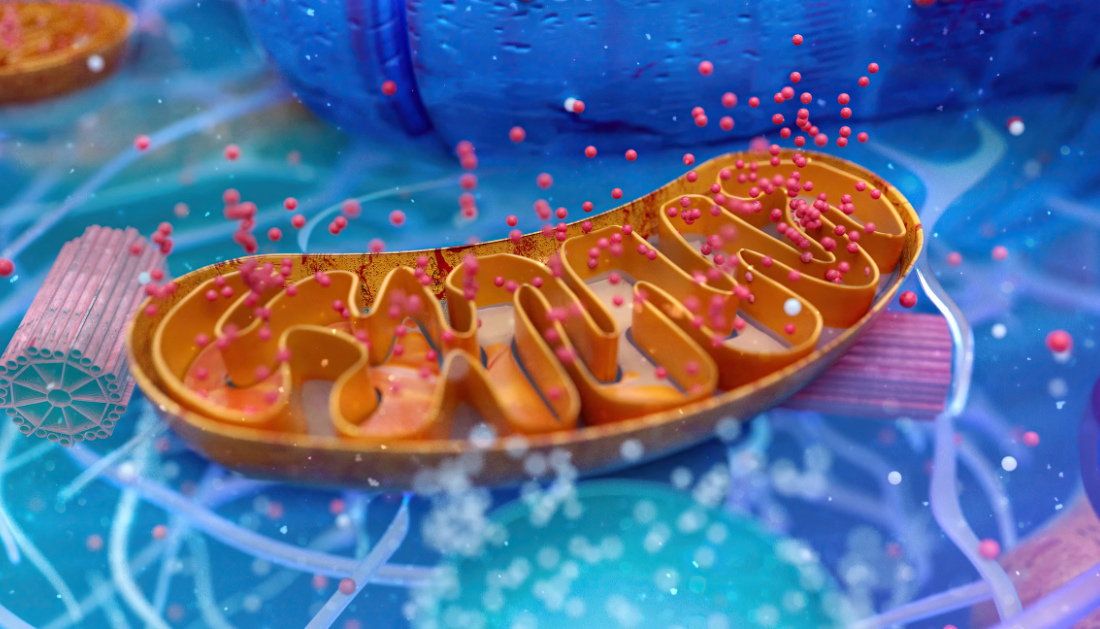
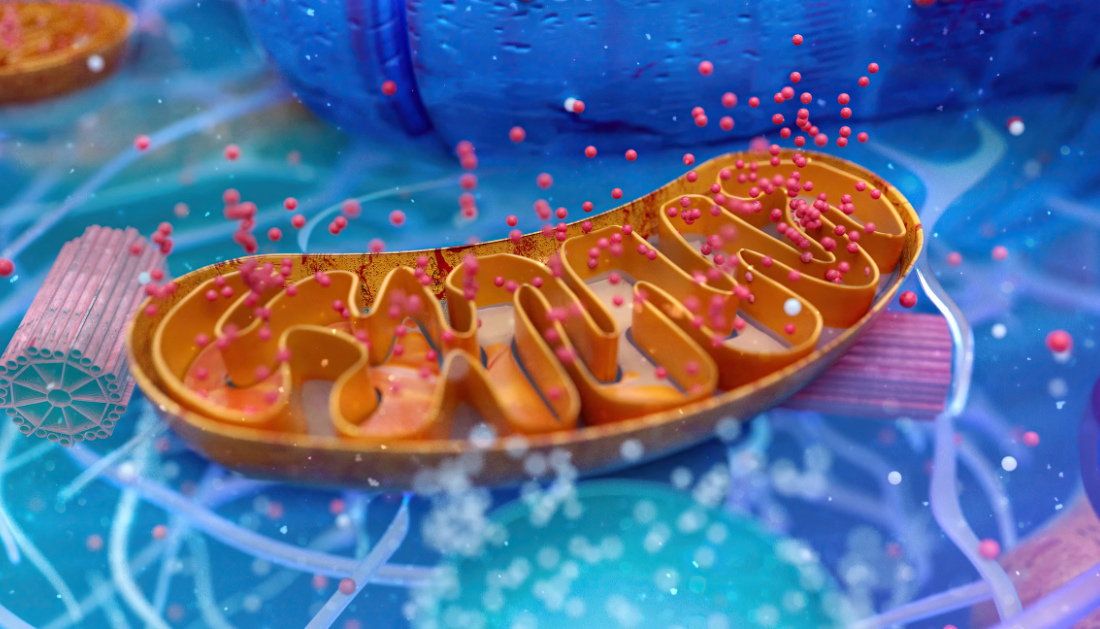
Scientists from the Cancer Research UK Scotland Institute and Memorial Sloan Kettering Cancer Center in the United States have “rewired” the DNA of mitochondria, which are energy producers found in all living cells. They discovered that making mutations in certain regions of this DNA impacts how effectively cancer responds to immunotherapy, which uses the body’s natural defenses to attack cancer cells.
This study opens up new avenues for identifying patients who would benefit the most from immunotherapy by looking for mitochondrial DNA abnormalities. Half of all malignancies contain mitochondrial DNA (mtDNA) mutations, and this study demonstrates for the first time that they can be used to improve cancer treatment.
In the future, combining medicines that mirror the effects of these mutations with immunotherapy may improve the chances of successful cancer treatment for multiple types.
In a publication titled “Mitochondrial DNA mutations drive aerobic glycolysis to enhance checkpoint blockade in melanoma,” published in Nature Cancer, scientists show for the first time a direct link between mitochondrial DNA (mtDNA) mutations and cancer therapy response. Surprisingly, scientists discovered that tumors with high levels of mtDNA mutations are up to 2.5 times more likely to respond to treatment with nivolumab, an immunotherapy medicine.
Nivolumab works by putting a “brake” on the immune system’s ability to assault cancer cells. It is being used to treat a variety of malignancies, including melanoma, lung cancer, liver cancer, and gastrointestinal cancer. The researchers anticipate that in the future, they might routinely test for mitochondrial DNA abnormalities, allowing clinicians to determine which patients will benefit the most from immunotherapy before beginning treatment.
DNA mutations may make treatment-resistant tumors susceptible to immunotherapy, allowing thousands more cancer patients to benefit from this groundbreaking treatment.
Cancer Research Horizons, Cancer Research UK’s innovation arm, has filed patent applications for the technologies that led to the finding. It will assist bring the technology to market, allowing for the development of new medicines that disrupt the energy sources used by cancer to spread and grow. To far, Cancer Research Horizons has introduced 11 novel cancer medications to the market, which have been used in over six million cancer treatment courses globally.
Dr. Payam Gammage, Group Leader at the Cancer Research UK Scotland Institute and the University of Glasgow, and co-lead author of the study, stated, “Cancer is a disease of our own bodies.”Cancer cells might appear to be healthy cells on the outside, making it difficult for human immune systems to recognize and destroy cancer cells.
For more information: Mitochondrial DNA mutations drive aerobic glycolysis to enhance checkpoint blockade in melanoma, Nature Cancer (2024). DOI: 10.1038/s43018-023-00721-w
more recommended stories
 Caffeine and SIDS: A New Prevention Theory
Caffeine and SIDS: A New Prevention TheoryFor the first time in decades,.
 Microbial Metabolites Reveal Health Insights
Microbial Metabolites Reveal Health InsightsThe human body is not just.
 Reelin and Cocaine Addiction: A Breakthrough Study
Reelin and Cocaine Addiction: A Breakthrough StudyA groundbreaking study from the University.
 Preeclampsia and Stroke Risk: Long-Term Effects
Preeclampsia and Stroke Risk: Long-Term EffectsPreeclampsia (PE) – a hypertensive disorder.
 Statins and Depression: No Added Benefit
Statins and Depression: No Added BenefitWhat Are Statins Used For? Statins.
 Azithromycin Resistance Rises After Mass Treatment
Azithromycin Resistance Rises After Mass TreatmentMass drug administration (MDA) of azithromycin.
 Generative AI in Health Campaigns: A Game-Changer
Generative AI in Health Campaigns: A Game-ChangerMass media campaigns have long been.
 Molecular Stress in Aging Neurons Explained
Molecular Stress in Aging Neurons ExplainedAs the population ages, scientists are.
 Higher BMI and Hypothyroidism Risk Study
Higher BMI and Hypothyroidism Risk StudyA major longitudinal study from Canada.
 Therapeutic Plasma Exchange Reduces Biological Age
Therapeutic Plasma Exchange Reduces Biological AgeTherapeutic plasma exchange (TPE), especially when.

Leave a Comment