Key Takeaways for HCPs
- Neutrophil activity follows a circadian rhythm that influences myocardial injury severity.
- A CXCR4–CXCL12 checkpoint shifts neutrophils into a protective “night-like” state.
- CXCR4 agonism limits inflammatory tissue damage without impairing host defence.
- Findings open new therapeutic directions for myocardial infarction and sterile inflammation.
Why Timing Matters in Post-MI Inflammation
Circadian control of neutrophils has emerged as a critical determinant of inflammatory injury after myocardial infarction (MI). In a study published in the Journal of Experimental Medicine, researchers identified a circadian immune checkpoint that regulates neutrophil activation and tissue positioning, significantly limiting collateral heart damage after ischemia-reperfusion injury.
Explore All Cardiology CME Conferences & Online Courses
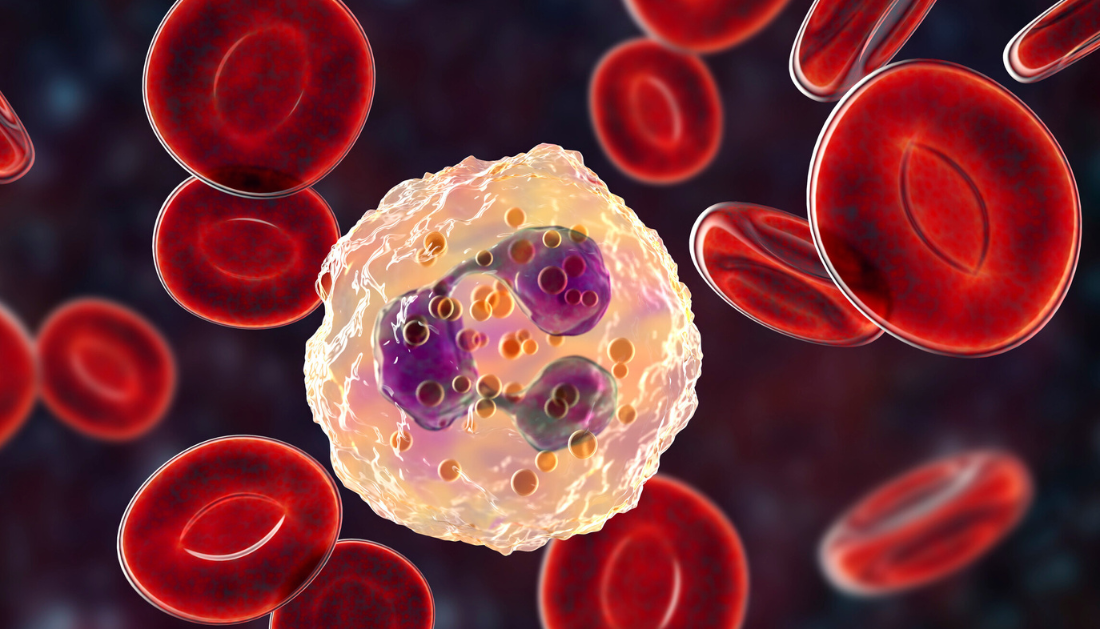
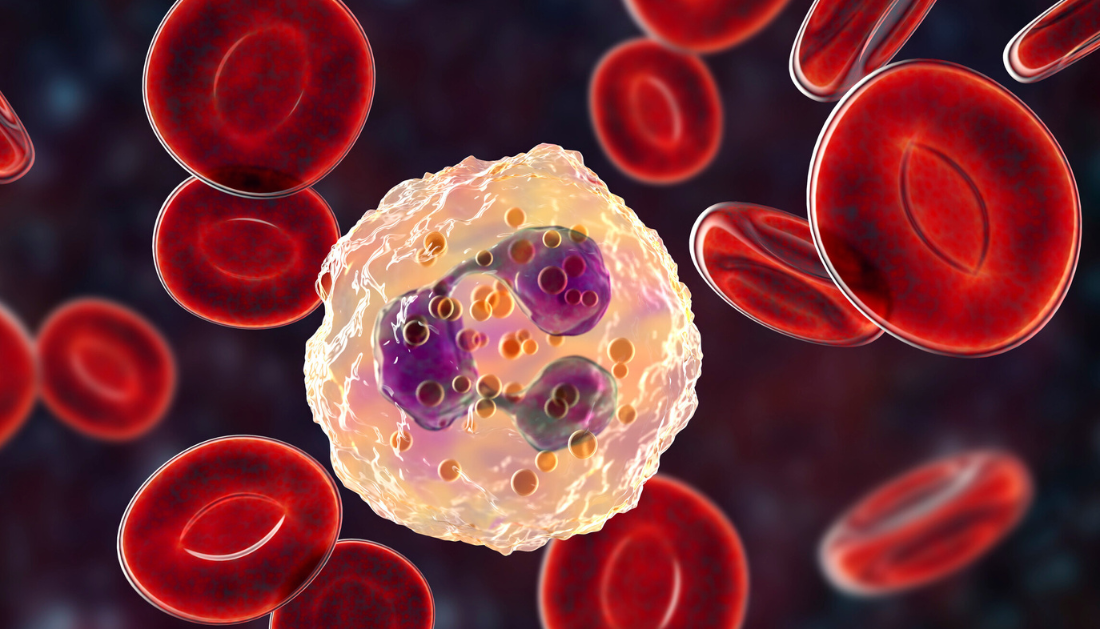
Neutrophils are essential first responders, but their cytotoxic activity can worsen sterile inflammation, particularly in cardiac tissue. The study highlights how neutrophil behaviour changes across the day-night cycle, offering a new lens through which to understand circadian patterns in myocardial injury observed in both experimental models and clinical settings.
How Circadian Control of Neutrophils Influences Cardiac Inflammation
Using a murine MI model, researchers demonstrated that infarct size varied markedly by time of day. Daytime ischemic injury resulted in larger infarcts, while nighttime injury was associated with reduced myocardial damage. Importantly, depleting neutrophils eliminated these circadian differences without affecting immune cell recruitment, underscoring neutrophils as key drivers of time-dependent injury.
Human data supported these findings. In a retrospective analysis of over 2,000 MI patients, higher neutrophil counts at admission correlated with increased troponin levels and more substantial diurnal variation in cardiac injury. Patients with lower neutrophil counts showed blunted or absent circadian injury patterns, reinforcing the link between neutrophils and myocardial damage.
Mechanistically, the neutrophil circadian clock, regulated by the transcription factor BMAL1, was shown to control basal activation states and intravascular behaviour. Disabling this clock protected mice from myocardial tissue death, even though systemic circadian rhythms remained intact.
Therapeutic Implications of Circadian Control of Neutrophils
The study identified CXCR4 and its ligand CXCL12 as a protective circadian checkpoint. Nighttime CXCL12 signalling through CXCR4 shifted neutrophils into a less damaging state. Pharmacologic activation of CXCR4 using the experimental agonist ATI2341 reproduced this effect, reducing myocardial injury and vascular inflammation without lowering neutrophil counts.
Notably, CXCR4 agonism repositioned neutrophils to injury sites while limiting spillover into healthy tissue, a natural nighttime defense mechanism. Crucially for clinicians, antimicrobial responses against Staphylococcus aureus and Candida albicans remained intact, addressing concerns about infection risk.
Clinical Relevance for Cardiovascular and Critical Care Teams
This discovery positions circadian neutrophil regulation as a promising therapeutic strategy for myocardial infarction, ischemia-reperfusion injury, and other inflammatory conditions. By selectively limiting neutrophil-mediated collateral damage, rather than suppressing immunity, CXCR4-targeted approaches may offer safer anti-inflammatory interventions aligned with circadian biology.
Source:
more recommended stories
 AI Predicts Chronic GVHD Risk After Stem Cell Transplant
AI Predicts Chronic GVHD Risk After Stem Cell TransplantKey Takeaways A new AI-driven tool,.
 Red Meat Consumption Linked to Higher Diabetes Odds
Red Meat Consumption Linked to Higher Diabetes OddsKey Takeaways Higher intake of total,.
 Pediatric Crohn’s Disease Microbial Signature Identified
Pediatric Crohn’s Disease Microbial Signature IdentifiedKey Points at a Glance NYU.
 Nanovaccine Design Boosts Immune Attack on HPV Tumors
Nanovaccine Design Boosts Immune Attack on HPV TumorsKey Highlights Reconfiguring peptide orientation significantly.
 High-Fat Diets Cause Damage to Metabolic Health
High-Fat Diets Cause Damage to Metabolic HealthKey Points Takeaways High-fat and ketogenic.
 Acute Ischemic Stroke: New Evidence for Neuroprotection
Acute Ischemic Stroke: New Evidence for NeuroprotectionKey Highlights A Phase III clinical.
 Statins Rarely Cause Side Effects, Large Trials Show
Statins Rarely Cause Side Effects, Large Trials ShowKey Points at a Glance Large.
 Can Too Many Antioxidants Harm Future Offspring?
Can Too Many Antioxidants Harm Future Offspring?Key Takeaways High-dose antioxidant supplementation in.
 Anxiety Reduction and Emotional Support on Social Media
Anxiety Reduction and Emotional Support on Social MediaKey Summary Anxiety commonly begins in.
 Liquid Biopsy Measures Epigenetic Instability in Cancer
Liquid Biopsy Measures Epigenetic Instability in CancerKey Takeaways Johns Hopkins researchers developed.

Leave a Comment