In a recent report published in the British Medical Journal, the researchers examined data on the diagnosis and treatment of heart failure.
Globally, heart failure has resulted in significant financial and health costs, particularly for the elderly. New scientific findings have led to the development of innovative medications and better heart failure patient outcomes. These include cutting-edge drugs, gadgets, and methods of diagnosis. Clinical standards take these advancements into account, yet often their recommendations for diagnosis and therapy need to be updated.
Concerning the review
Researchers provide updated information on heart failure management in this review.
The Cochrane and PubMed databases were combed for randomized clinical trials (RCTs), epidemiological studies, and cohort studies about the diagnosis and management of heart failure that were published between January 2015 and July 7, 2023. They included studies that were not included in the 2021–2022 guidelines of the European Society of Cardiology (ESC) and the Heart Failure Society of America/American College of Cardiology/American Heart Association (HFSA/ACC/AHA), which didn’t include case reports and case series.
The diagnosis and epidemiology of heart failure
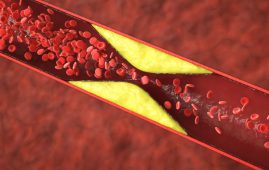
According to the Global Burden of Disease (GBD) study, 57 million people experienced heart failure episodes in 2019. Age-standardized rates decreased from 7.70 per 1,000 to 7.10 per 1,000 between 2010 and 2019. The rates, however, are not linear; from 2016 to 2019, there will be annual growth of 0.6% after initial declines. Young people are being admitted to hospitals in the US at a higher rate due to heart failure. After diagnosis, the odds of survival are low and largely influenced by age. The use of life-prolonging medications, sodium-glucose cotransporter-2 (SGL-2) inhibitors, and basic drug groups has increased in heart failure care.
Heart failure is defined as cardiac dysfunction, reduced left ventricular systolic function (≤40%), or increased filling pressures. Heart failures with reduced ejection fractions (HFrEF), heart failures with minimally reduced ejection fractions (HFmrEF), and heart failures with preserved ejection fractions (HFpEF) are the three categories based on the left ventricular ejection fraction (LVEF).
It is difficult to diagnose HFpEF because of the difficulty in recognizing elevated filling pressure. While invasive techniques are the best way to detect elevated filling pressures in the left ventricle, non-invasive diagnosis can also be made using clinical scores like HFA-PEFF and H2FPEF. Determining the cause of heart failure is essential since certain conditions call for specific treatment. People with significantly hypertrophic arteries on echocardiography and dilated cardiomyopathies can benefit from cardiac magnetic resonance imaging (CMR) studies.
Improvements in the treatment of heart failure
Renin-angiotensin system (RAS) inhibitors, SGLT2 inhibitors, angiotensin receptor blocking agents (ARBs), angiotensin receptor/neprilysin inhibitor molecules (ARNI), β blockers, mineralocorticoid receptor antagonist medications (MRAs) are prescribed to patients with HFrEF. as these four HFrEF medication pillars are combined, the relative risk of death can be lowered by 73%, and the number needed to treat (NNT) can be decreased to prevent death as compared to not receiving treatment.
One of the mainstays of heart failure management is combined ARB and ARNI medication. The SGL-2 inhibitor family was created to improve diabetes-related glucose control and can optimize cardiac outcomes, including the prevention of heart failure. These days, dapagliflozin and empagliflozin are part of this class, which is thought to be one of the four main drugs used to prevent diabetes and heart failure. About 15% of patients with heart failure will see a gain in left ventricular function (LVEF) from less than 40% to more than 40% during follow-up. The initial course of treatment for people with slightly reduced or sustained LVEF is SGLT2 inhibitors. ARBs, MRAs, ARNI, and ACE inhibitors are some additional treatments for HFrEF; however, because of their lack of efficacy, they are regarded as second-line therapy.
For African Americans with NYHA class III or IV heart failure, the African-American Heart Failure Trial recommends a combination of medications. Ivabradine, a cardiac pacemaker current inhibitor, decreased hospital admissions and cardiovascular mortality by 18% in patients with sinus rhythm and heart rates ≥70 bpm. Vericiguat, a new medication for heart failure that decreases cardiac remodeling and enhances vasodilation, decreased the risk of cardiovascular death or hospital admission by 10% in the VICTORIA research.
Implanted cardiac defibrillators (ICDs) and cardiac resynchronization therapy (CRT) are two components of heart failure resynchronization treatment (HFrEF). When deciding on an ICD implantation together, healthcare providers need to take into account the preferences of each patient as well as any prospective benefits. Patients with severe, chronic mitral regurgitation may benefit from transcatheter edge-to-edge repair (TEER).
The review’s conclusions indicate that the introduction of four life-prolonging drug classes for people with low LVEF and SGLT2 inhibitors for people with moderately decreased and maintained LVEF has significantly altered the care of heart failure patients. Still, getting the right diagnosis is not easy. To determine the best way to begin and what factors influence the fluctuations in the prevalence of heart failure, more research is required. Additionally, studies should look into the benefits of medications for preserving LVEF and whether or not patients should stop taking them if their symptoms get better and their left ventricular function gets back to normal.
For more information: Advances in management of heart failure, BMJ, doi: https://doi.org/10.1136/bmj-2023-077025
more recommended stories
 Children’s Health in the United States is Declining!
Children’s Health in the United States is Declining!Summary: A comprehensive analysis of U.S..
 Autoimmune Disorders: ADA2 as a Therapeutic Target
Autoimmune Disorders: ADA2 as a Therapeutic TargetAdenosine deaminase 2 (ADA2) has emerged.
 Is Prediabetes Reversible through Exercise?
Is Prediabetes Reversible through Exercise?150 Minutes of Weekly Exercise May.
 New Blood Cancer Model Unveils Drug Resistance
New Blood Cancer Model Unveils Drug ResistanceNew Lab Model Reveals Gene Mutation.
 Healthy Habits Slash Diverticulitis Risk in Half: Clinical Insights
Healthy Habits Slash Diverticulitis Risk in Half: Clinical InsightsHealthy Habits Slash Diverticulitis Risk in.
 Caffeine and SIDS: A New Prevention Theory
Caffeine and SIDS: A New Prevention TheoryFor the first time in decades,.
 Microbial Metabolites Reveal Health Insights
Microbial Metabolites Reveal Health InsightsThe human body is not just.
 Reelin and Cocaine Addiction: A Breakthrough Study
Reelin and Cocaine Addiction: A Breakthrough StudyA groundbreaking study from the University.
 Preeclampsia and Stroke Risk: Long-Term Effects
Preeclampsia and Stroke Risk: Long-Term EffectsPreeclampsia (PE) – a hypertensive disorder.
 Statins and Depression: No Added Benefit
Statins and Depression: No Added BenefitWhat Are Statins Used For? Statins.

Leave a Comment