

“Our study shows that the cellular mechanisms of cancer’s self-preservation, when sufficiently understood, can be used against the disease very effectively. I look forward to future research on metabolism-driven mechanisms of immunosuppression in glioblastoma, and I’m hopeful for all that we will continue to learn about how to best understand and fight this cancer.” -Dr. Filippo Veglia, Ph.D., Assistant Professor, The Wistar Institute
The mechanism by which monocyte-derived macrophages and microglia produce an immunosuppressive tumor microenvironment in glioblastoma has not been well understood up until now. When glioblastoma developed, monocyte-derived macrophages began to outnumber microglia. This finding suggested that the cancer’s eventual goal of evading the immune response was aided by the monocyte-derived macrophages’ eventual majority status in the tumor microenvironment. The Veglia lab examined the cellular “how” of glioblastoma immunosuppression. In fact, in preclinical models and patients, monocyte-derived macrophages, but not microglia, inhibited the function of T cells—immune cells that kill tumor cells. When the researchers examined preclinical glioblastoma models with artificially lowered levels of monocyte-derived macrophages, they were able to corroborate this discovery. Additionally, the models with fewer harmful macrophages in the tumor microenvironment performed better than the conventional glioblastoma models, as predicted by the group.
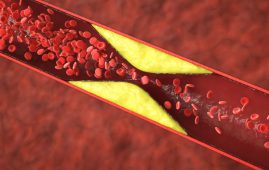
Immunosuppression plays a critical role in glioblastoma’s aggressiveness. Due to its location in the brain and this immunosuppression, the tumor microenvironment is particularly hazardous and resistant to immunotherapy. This harsh reality is reflected in the dire prognosis for patients, with only 25% surviving more than a year after diagnosis. The cancer actively manipulates immune cells like macrophages, turning them into allies that promote tumor growth and evade the body’s defenses.
The Veglia team then set out to determine the precise mechanism by which the immune cells associated with cancer were suppressing the immune system after confirming the function of monocyte-derived macrophages. To determine which gene(s) might be responsible for immunosuppression, the researchers sequenced the macrophages in question. They also looked into the metabolic patterns of the macrophages to determine whether the abnormal gene expression of the cells was related to metabolism.
The team discovered glucose metabolism using metabolic studies and twin gene expression. The Veglia group was able to ascertain through a battery of experiments that monocyte-derived macrophages expressing GLUT1, a significant transporter for glucose (a crucial metabolic molecule) and having improved glucose metabolism, inhibited T cell activity by secreting interleukin-10 (IL-10). The researchers showed that the immunosuppressive activity of these macrophages was caused by impaired glucose metabolism brought on by glioblastoma.
The researchers found that a process known as “histone lactylation” is responsible for the immunosuppressive potency of macrophages that are driven by glucose metabolism. The structural proteins called histones are important in determining the conditions in which some genes, such as IL-10, are produced. Lactate is a byproduct of glucose metabolism produced by monocyte-derived macrophages, which are fast glucose-metabolizing cells. Additionally, histones can become “lactylated” (lactate incorporated into histones) in a way that further enhances the organization of histones and stimulates the synthesis of IL-10, which is efficiently produced by macrophages originating from monocytes to aid in the growth of cancer cells.
However, how might the glucose-induced immunosuppressive function of macrophages generated from monocytes be inhibited? A potential remedy was discovered by Dr. Veglia and his research group: PERK, an enzyme that controls GLUT1 expression in macrophages and glucose metabolism. Targeting PERK decreased the immunosuppressive activity of macrophages and histone lactylation in preclinical models of glioblastoma; when combined with immunotherapy, this prevented cancer from progressing and created long-lasting immunity that shielded the brain from tumor regrowth. These findings suggest that targeting the PERK-histone lactylation axis could be a useful tactic in the fight against this deadly brain cancer.
For more information: Glucose-driven histone lactylation promotes the immunosuppressive activity of monocyte-derived macrophages in glioblastoma, Immunity, doi.org/10.1016/j.immuni.2024.04.006
more recommended stories
 New Blood Cancer Model Unveils Drug Resistance
New Blood Cancer Model Unveils Drug ResistanceNew Lab Model Reveals Gene Mutation.
 Healthy Habits Slash Diverticulitis Risk in Half: Clinical Insights
Healthy Habits Slash Diverticulitis Risk in Half: Clinical InsightsHealthy Habits Slash Diverticulitis Risk in.
 Caffeine and SIDS: A New Prevention Theory
Caffeine and SIDS: A New Prevention TheoryFor the first time in decades,.
 Microbial Metabolites Reveal Health Insights
Microbial Metabolites Reveal Health InsightsThe human body is not just.
 Reelin and Cocaine Addiction: A Breakthrough Study
Reelin and Cocaine Addiction: A Breakthrough StudyA groundbreaking study from the University.
 Preeclampsia and Stroke Risk: Long-Term Effects
Preeclampsia and Stroke Risk: Long-Term EffectsPreeclampsia (PE) – a hypertensive disorder.
 Statins and Depression: No Added Benefit
Statins and Depression: No Added BenefitWhat Are Statins Used For? Statins.
 Azithromycin Resistance Rises After Mass Treatment
Azithromycin Resistance Rises After Mass TreatmentMass drug administration (MDA) of azithromycin.
 Generative AI in Health Campaigns: A Game-Changer
Generative AI in Health Campaigns: A Game-ChangerMass media campaigns have long been.
 Molecular Stress in Aging Neurons Explained
Molecular Stress in Aging Neurons ExplainedAs the population ages, scientists are.

Leave a Comment