Poor kidney function may influence levels of Alzheimer’s biomarkers, but not necessarily dementia risk, according to new findings published in Neurology. This association is clinically essential for neurologists, nephrologists, geriatricians, and frontline HCPs interpreting blood-based Alzheimer’s diagnostics.
Explore All Neurology CME/CE Conferences and Online Courses
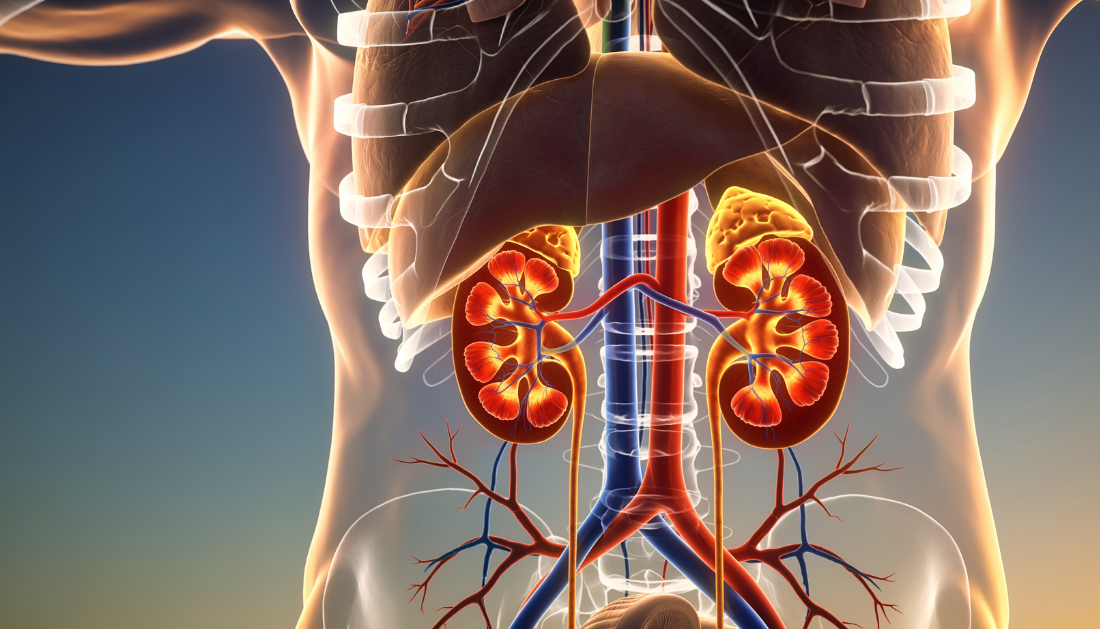
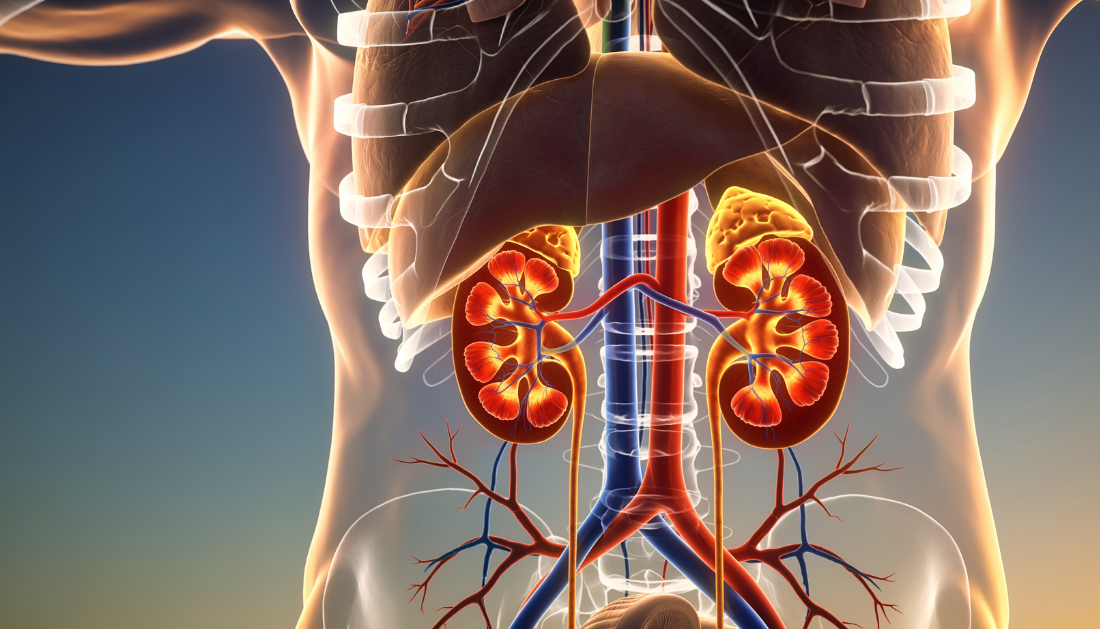
Growing Clinical Attention: Kidney Health and Alzheimer’s Biomarkers
Researchers analyzed 2,279 adults (average age 72) without dementia at baseline. They found that individuals with reduced kidney function showed higher levels of tau, amyloid beta, neurofilament light chain (NfL), and glial fibrillary acidic protein. These results held even after excluding early dementia cases.
Because kidneys filter waste and proteins from the bloodstream, impaired function may allow biomarkers to accumulate, leading to higher readings despite no actual increase in neurodegenerative burden.
Explore All Nephrology CME/CE Conferences and Online Courses
Study author Francesca Gasparini, MD, emphasized that clinicians should consider renal health as a vital variable when interpreting Alzheimer’s blood tests, especially in older adults or those with comorbidities.
Clinical Insight: Dementia Risk vs. Dementia Timing
After adjusting for age, sex, and APOEe4 status, poor kidney function was not associated with a higher likelihood of developing dementia.
However, a key interaction emerged:
Patients with impaired kidney function and elevated NfL levels had nearly double the risk of developing dementia compared to those with preserved renal function but similarly high biomarker levels.
This suggests kidney health may influence when dementia develops, rather than if it occurs, in patients already showing biomarker elevations.
Implications for HCPs: Interpretation, Monitoring & Follow-Up
These findings highlight an emerging diagnostic principle:
“Why Kidney Screening Matters in Alzheimer’s Blood Testing”
Monitoring renal function may help prevent misinterpretation of elevated biomarkers and support more accurate risk stratification.
A key limitation is that biomarkers were measured only once, and the cohort primarily included highly educated urban Swedish adults, limiting generalizability. Still, the study underscores the diagnostic value of a combined neurology–nephrology view for older patients undergoing dementia screening.
Source:
more recommended stories
 CTNNB1 Syndrome Study Explores Beta-Catenin Defects
CTNNB1 Syndrome Study Explores Beta-Catenin DefectsKey Takeaways Researchers in Spain are.
 Tuberculosis Breakthrough with Experimental Antibiotics
Tuberculosis Breakthrough with Experimental AntibioticsKey Takeaways Experimental antibiotics disrupt a.
 National Healthy Longevity Trial Receives Federal Support
National Healthy Longevity Trial Receives Federal SupportKey Summary Up to $38 million.
 Vascular Health Linked to Early Alzheimer’s Brain Changes
Vascular Health Linked to Early Alzheimer’s Brain ChangesKey Takeaways Brain vascular health is.
 Red Blood Cells Improve Glucose Tolerance Under Hypoxia
Red Blood Cells Improve Glucose Tolerance Under HypoxiaKey Takeaways for Clinicians Chronic hypoxia.
 Nanoplastics in Brain Tissue and Neurological Risk
Nanoplastics in Brain Tissue and Neurological RiskKey Takeaways for HCPs Nanoplastics are.
 AI Predicts Chronic GVHD Risk After Stem Cell Transplant
AI Predicts Chronic GVHD Risk After Stem Cell TransplantKey Takeaways A new AI-driven tool,.
 Red Meat Consumption Linked to Higher Diabetes Odds
Red Meat Consumption Linked to Higher Diabetes OddsKey Takeaways Higher intake of total,.
 Pediatric Crohn’s Disease Microbial Signature Identified
Pediatric Crohn’s Disease Microbial Signature IdentifiedKey Points at a Glance NYU.
 Nanovaccine Design Boosts Immune Attack on HPV Tumors
Nanovaccine Design Boosts Immune Attack on HPV TumorsKey Highlights Reconfiguring peptide orientation significantly.

Leave a Comment